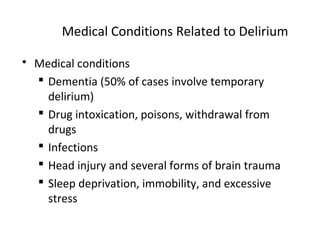
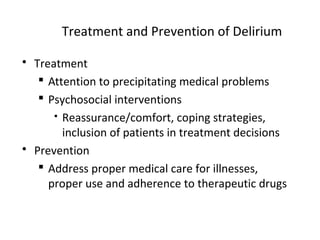
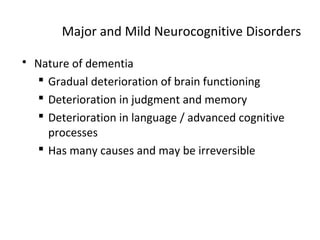
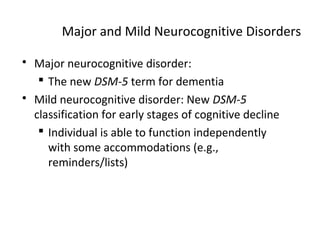
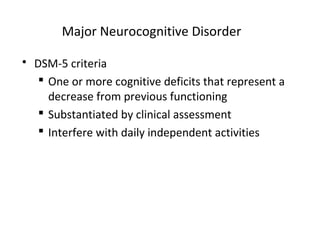
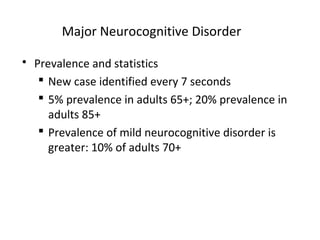
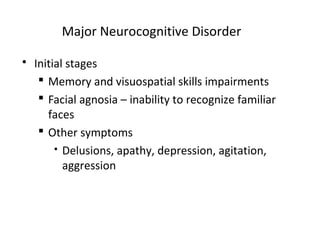
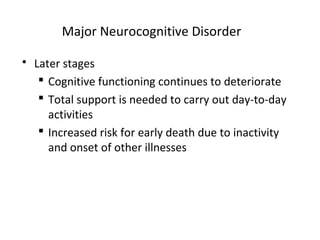
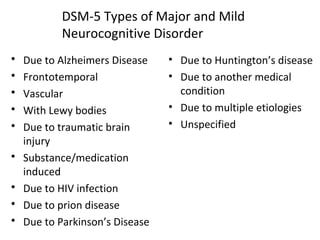
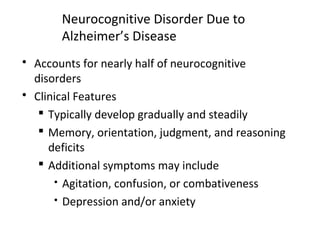
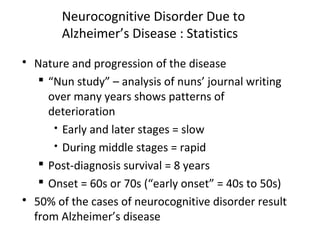
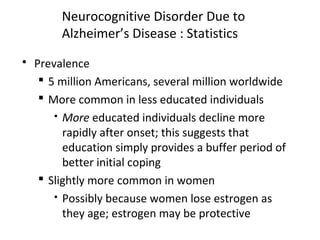
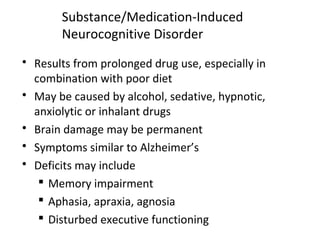
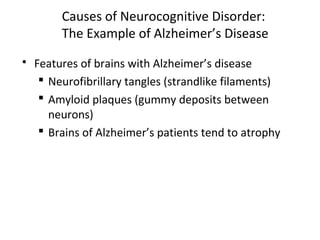
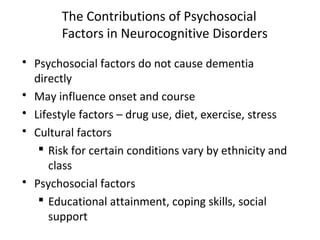
Neurocognitive disorders affect learning, memory, and consciousness. They range from temporary conditions like delirium to long-term disorders like dementia. While some may be caused by medical conditions or drug use, the most common types like Alzheimer's disease and vascular dementia develop due to aging and brain changes. Treatments aim to slow progression but cannot stop deterioration of cognitive skills. Lifestyle factors and social support may influence the course of disorders, but prevention is difficult as risk is determined by genetics in many cases.




![[INSERT Table 15.2 HERE, p. 556]](https://image.slidesharecdn.com/neurocognitivedisorders1-151129173124-lva1-app6892/85/Neurocognitive-disorders-1-20-320.jpg)
![[INSERT Figure 15.1 HERE, p. 548]](https://image.slidesharecdn.com/neurocognitivedisorders1-151129173124-lva1-app6892/85/Neurocognitive-disorders-1-23-320.jpg)
![[INSERT Table 15.1 HERE, p. 550]](https://image.slidesharecdn.com/neurocognitivedisorders1-151129173124-lva1-app6892/85/Neurocognitive-disorders-1-25-320.jpg)
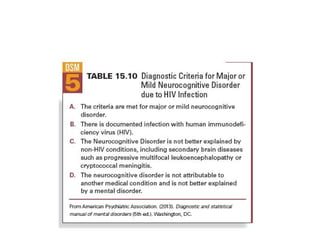
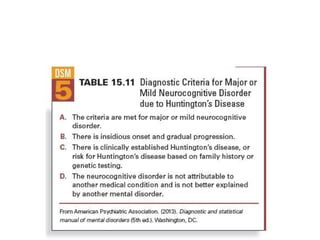
![[INSERT Disorder Criteria Summary, Major or Mild
Vascular Neurocognitive Disorder HERE, p. 552]](https://image.slidesharecdn.com/neurocognitivedisorders1-151129173124-lva1-app6892/85/Neurocognitive-disorders-1-28-320.jpg)




![[INSERT Table 15.4 HERE, p. 563]](https://image.slidesharecdn.com/neurocognitivedisorders1-151129173124-lva1-app6892/85/Neurocognitive-disorders-1-54-320.jpg)