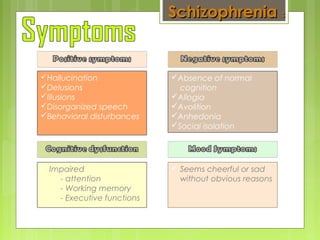
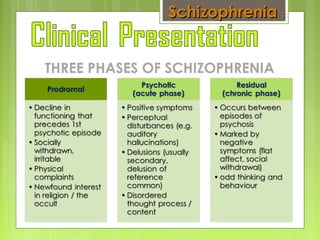
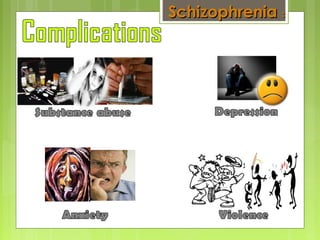
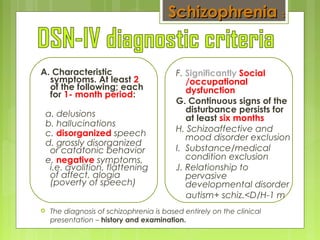
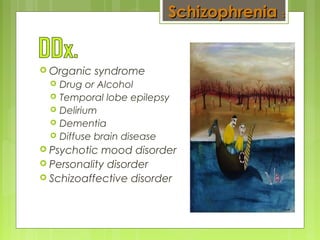
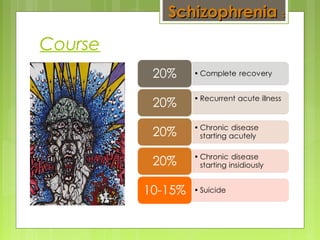
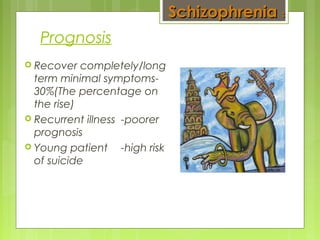
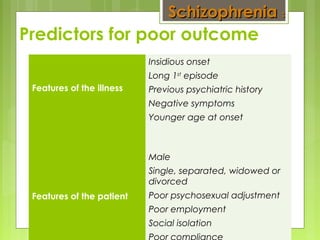
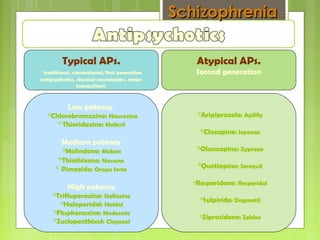
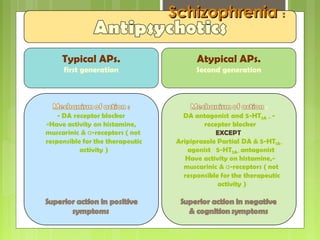
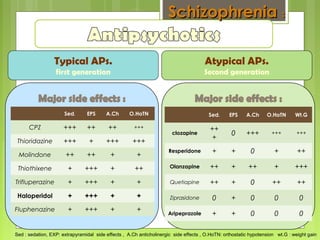
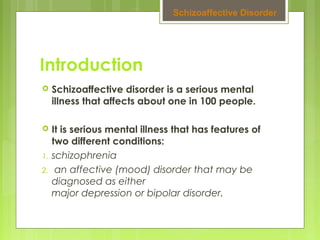
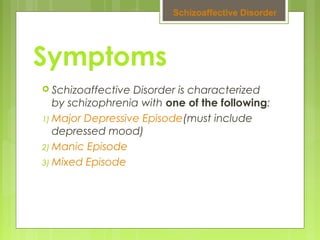
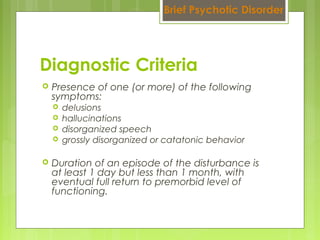
Schizophrenia is a severe mental illness characterized by distortions in thinking, perception, emotions, and behavior. It affects about 1% of the population and is one of the most challenging diseases in medicine. The causes are unknown but may involve genetic and environmental factors. Symptoms include hallucinations, delusions, disorganized speech and behavior, and decreased emotional expression and motivation. Treatment involves antipsychotic medications and psychotherapy. The prognosis is varied, with about 30% recovering fully and others experiencing recurrent symptoms.