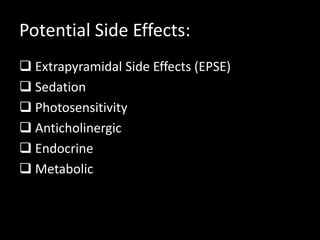
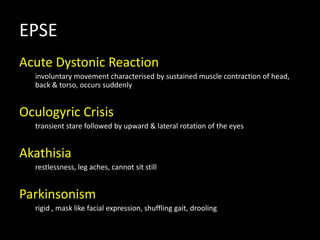
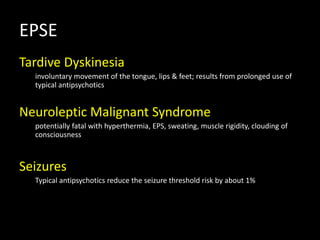
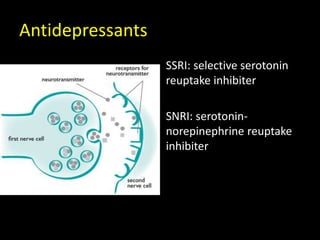
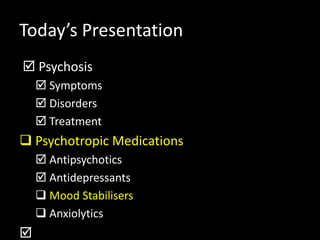
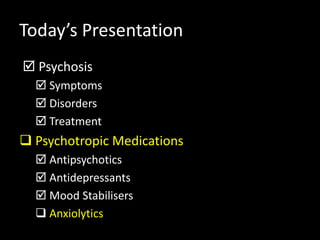
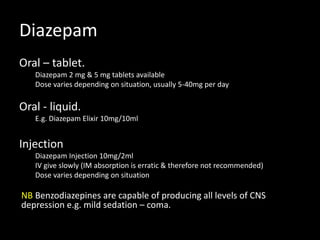
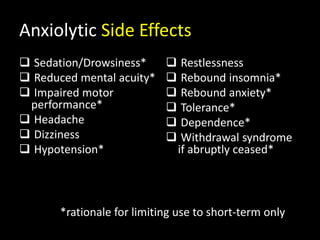
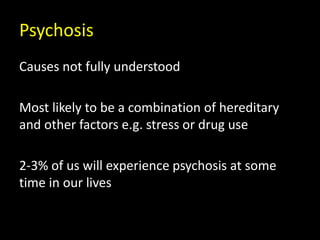
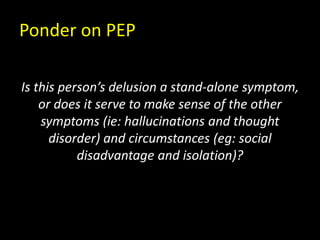
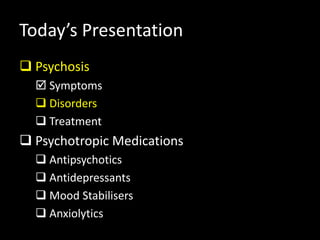
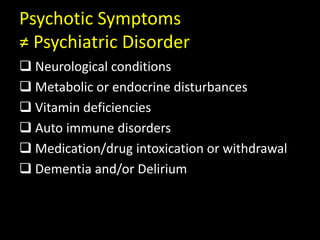
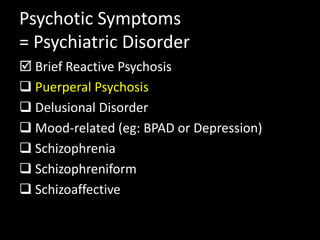
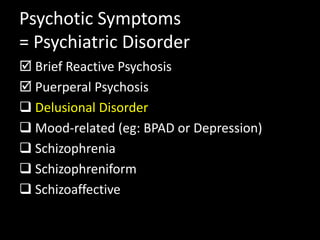
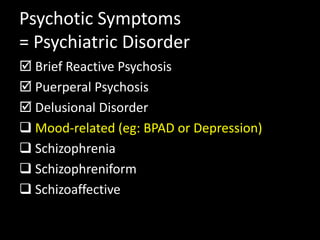
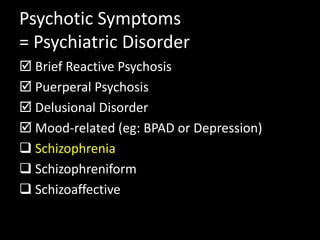
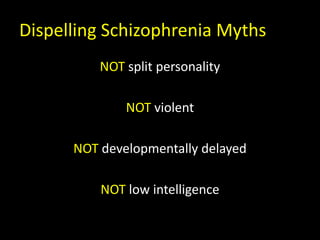
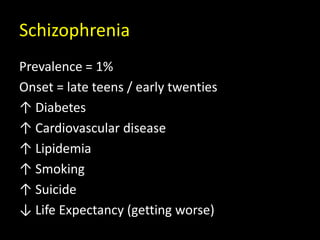
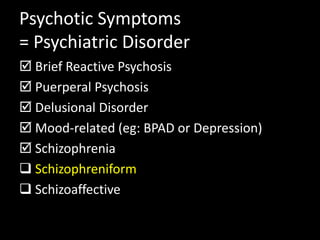
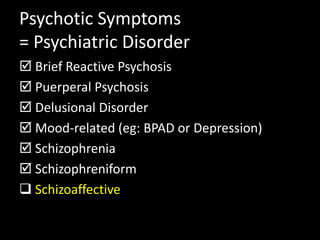
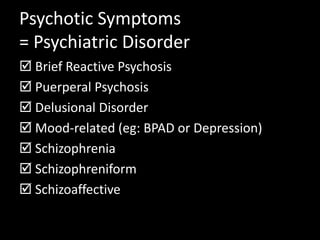
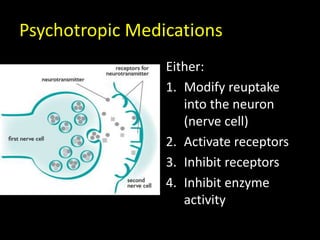
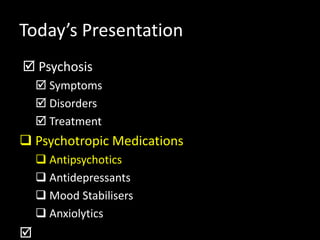
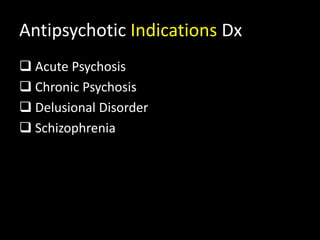
This document provides an overview of psychosis and psychotic disorders, their symptoms, and treatment including psychotropic medications. It discusses key psychotic symptoms like hallucinations, delusions, and thought disorders. It also outlines several psychiatric disorders that involve psychosis such as brief reactive psychosis, schizophrenia, and schizoaffective disorder. The document reviews treatment approaches for psychosis including supportive psychotherapy, cognitive behavioral therapy, and the use of psychotropic medications like antipsychotics.
![Schizophrenia
“a [group of] disorder[s] characterised by a
major disturbance in thought, perception,
cognition and psychosocial functioning”
Elder, Evans & Nizette (2013) pp 525 + 265](https://image.slidesharecdn.com/session4lecture-150116193335-conversion-gate01/85/Psychosis-and-Psychotropic-Meds-28-320.jpg)
![Positive & Negative Symptoms
+ve [excess]
Hallucinations
Delusions
Thought Disorder
-ve [deficit]
Avolition (↓ drive)
Anergia (↓ energy)
Anhedonia (↓ pleasure)
Affect Blunted
Alogia (↓ speech)](https://image.slidesharecdn.com/session4lecture-150116193335-conversion-gate01/85/Psychosis-and-Psychotropic-Meds-38-320.jpg)

![Antipsychotic Indications Sx
+ve [excess]
Hallucinations
Delusions
Thought Disorder
-ve [deficit]
Avolition (↓ drive)
Anergia (↓ energy)
Anhedonia (↓ pleasure)
Affect Blunted
Alogia (↓ speech)](https://image.slidesharecdn.com/session4lecture-150116193335-conversion-gate01/85/Psychosis-and-Psychotropic-Meds-56-320.jpg)