The document outlines learning objectives and provides information about schizophrenia, including:
- Risk factors include genetic and environmental factors such as family history and obstetric complications.
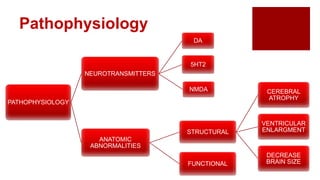
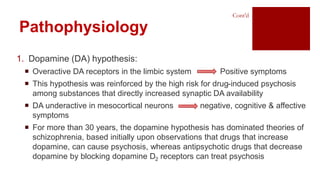
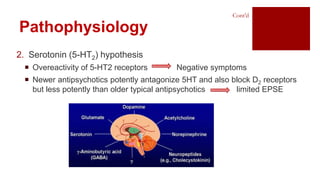
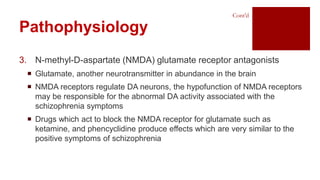
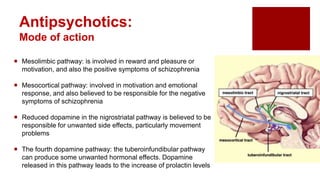
- Pathophysiology may involve dopamine, serotonin, and NMDA receptor abnormalities and structural brain changes.
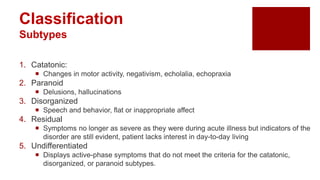
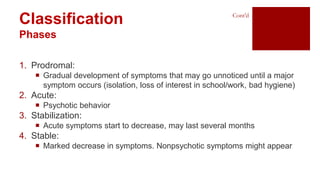
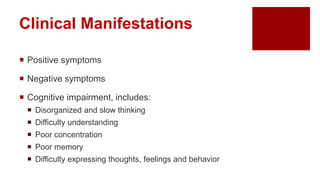
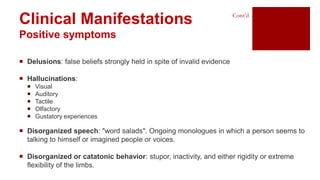
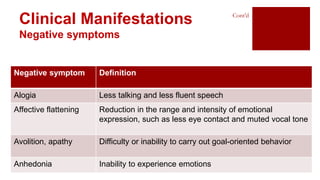
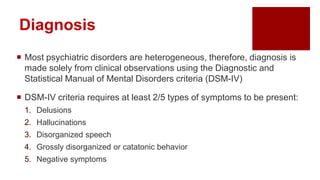
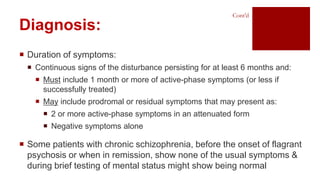
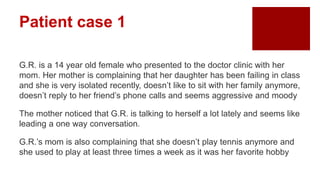
- Symptoms include positive symptoms like delusions and hallucinations, and negative symptoms such as reduced speech.
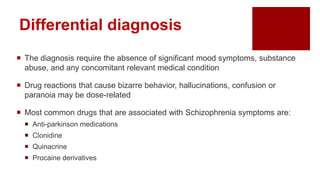
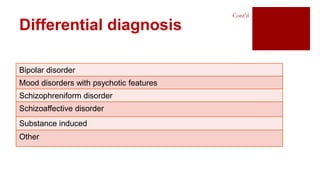
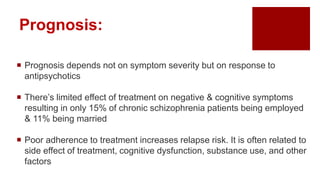
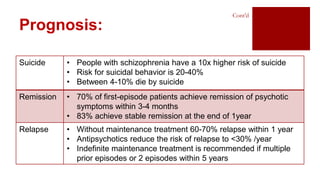
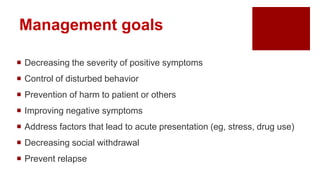
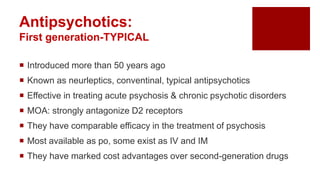
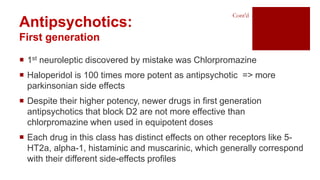
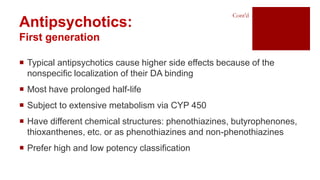
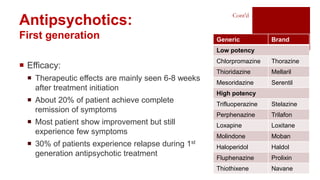
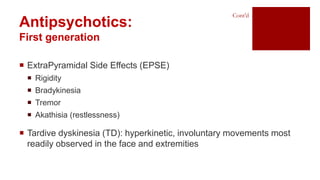
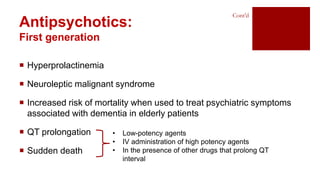
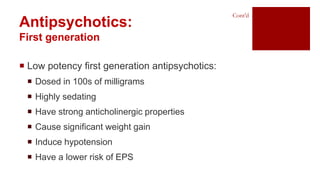
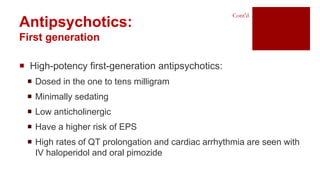
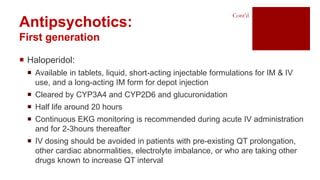
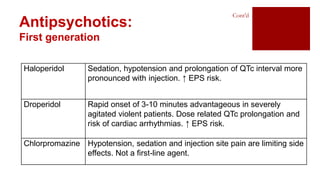
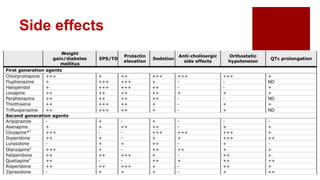
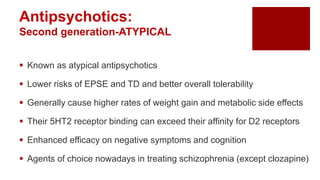
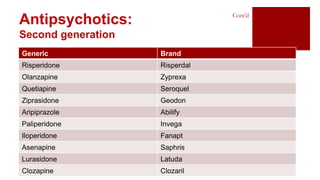
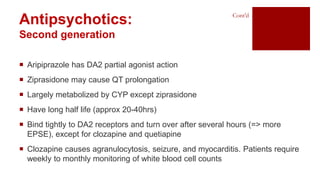
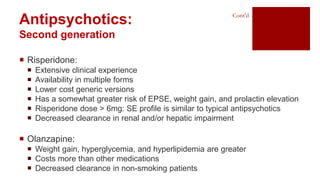
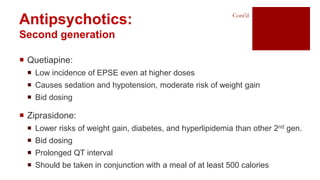
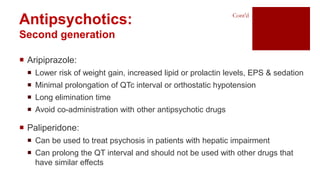
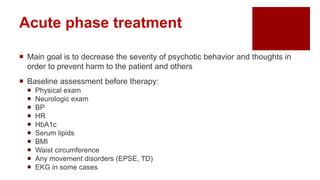
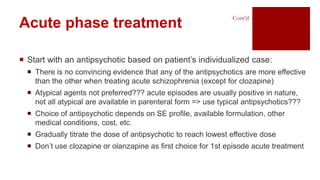
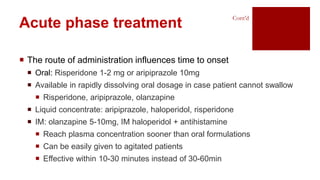
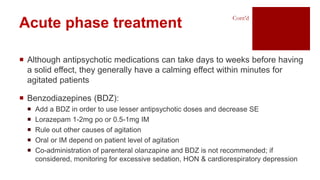
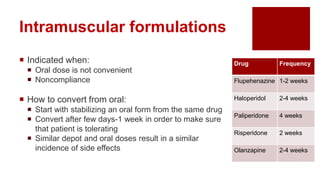
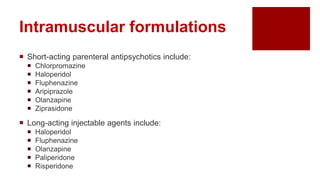
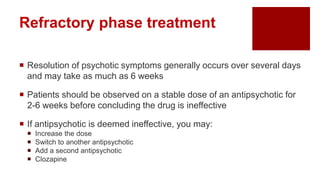
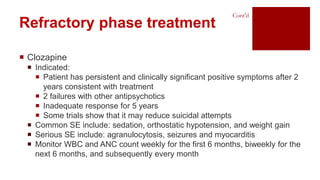
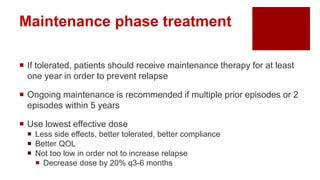
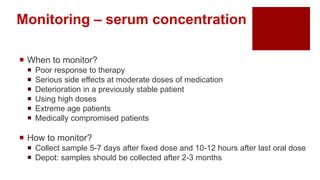
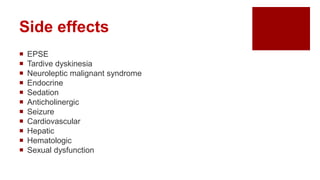
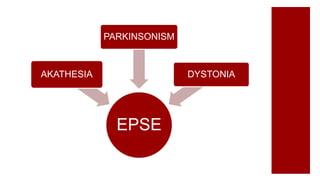
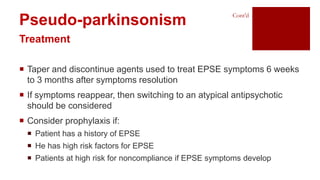
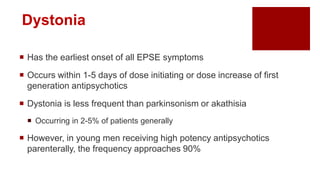
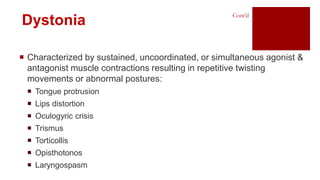
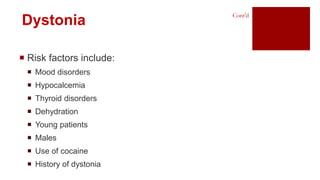
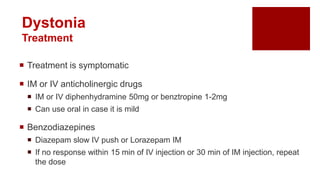
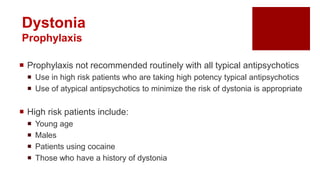
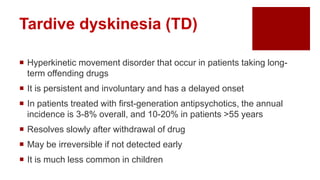
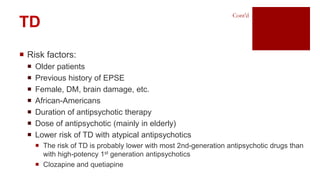
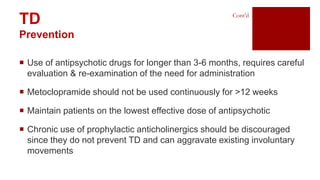
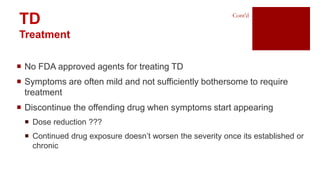
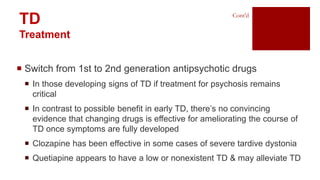
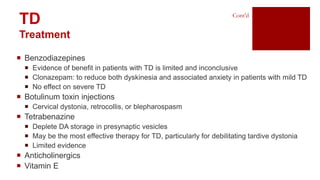
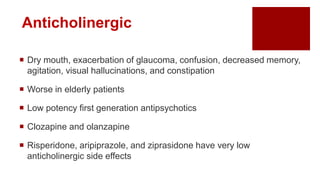
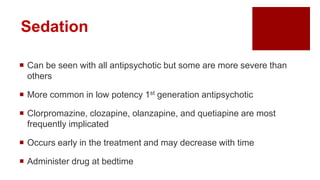
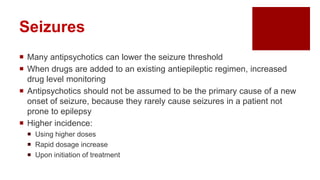
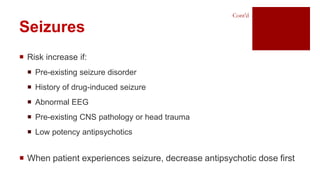
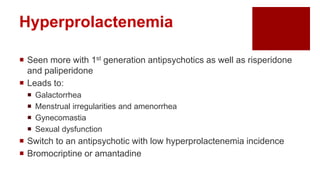
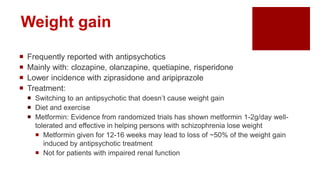
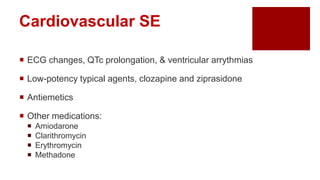
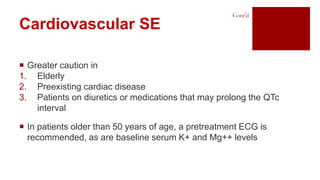
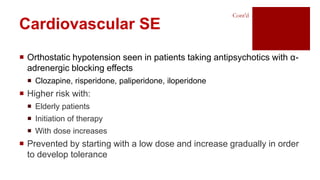
- Treatment involves antipsychotic drugs to reduce positive symptoms as well as managing side effects and preventing relapse.