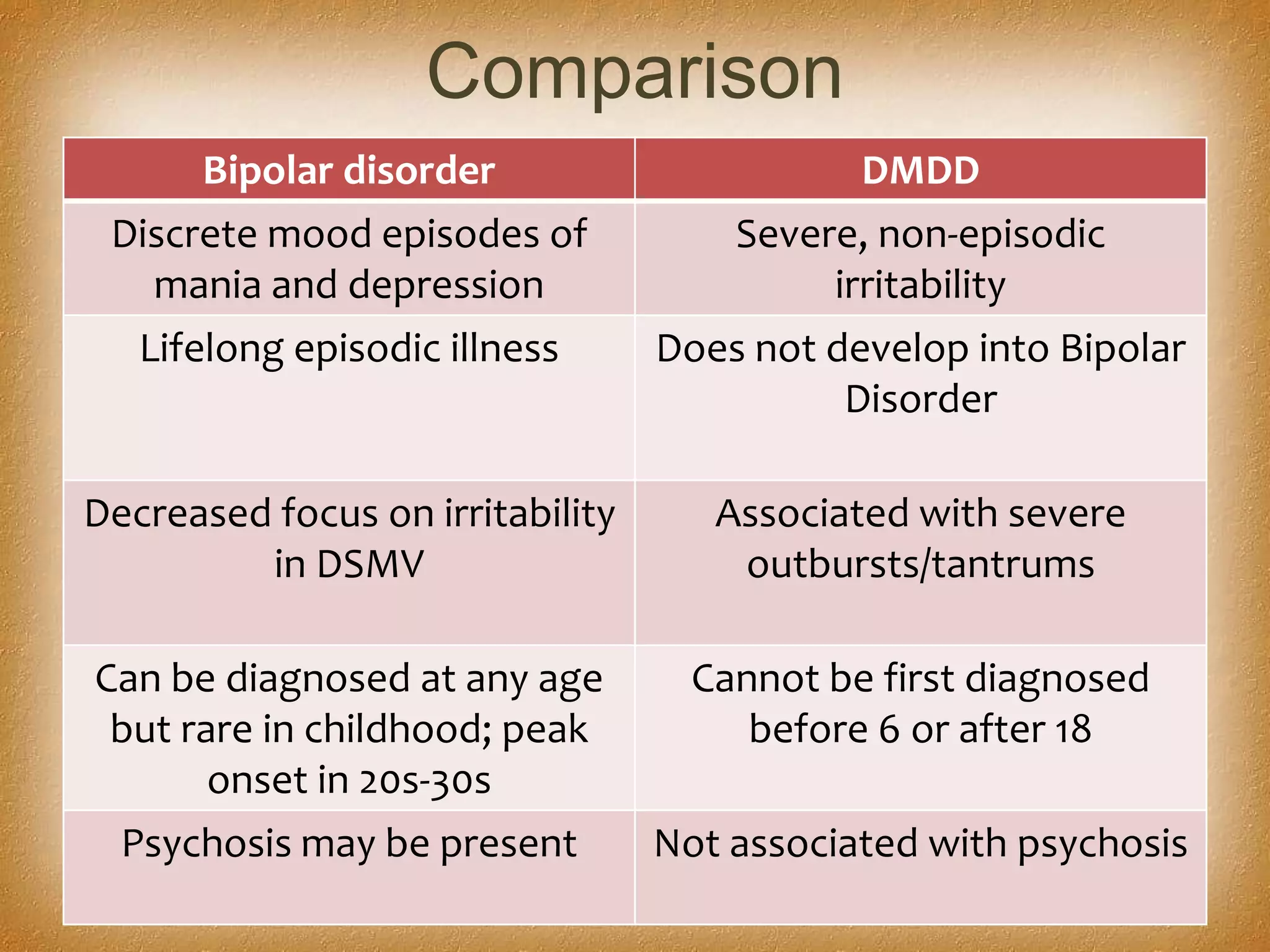
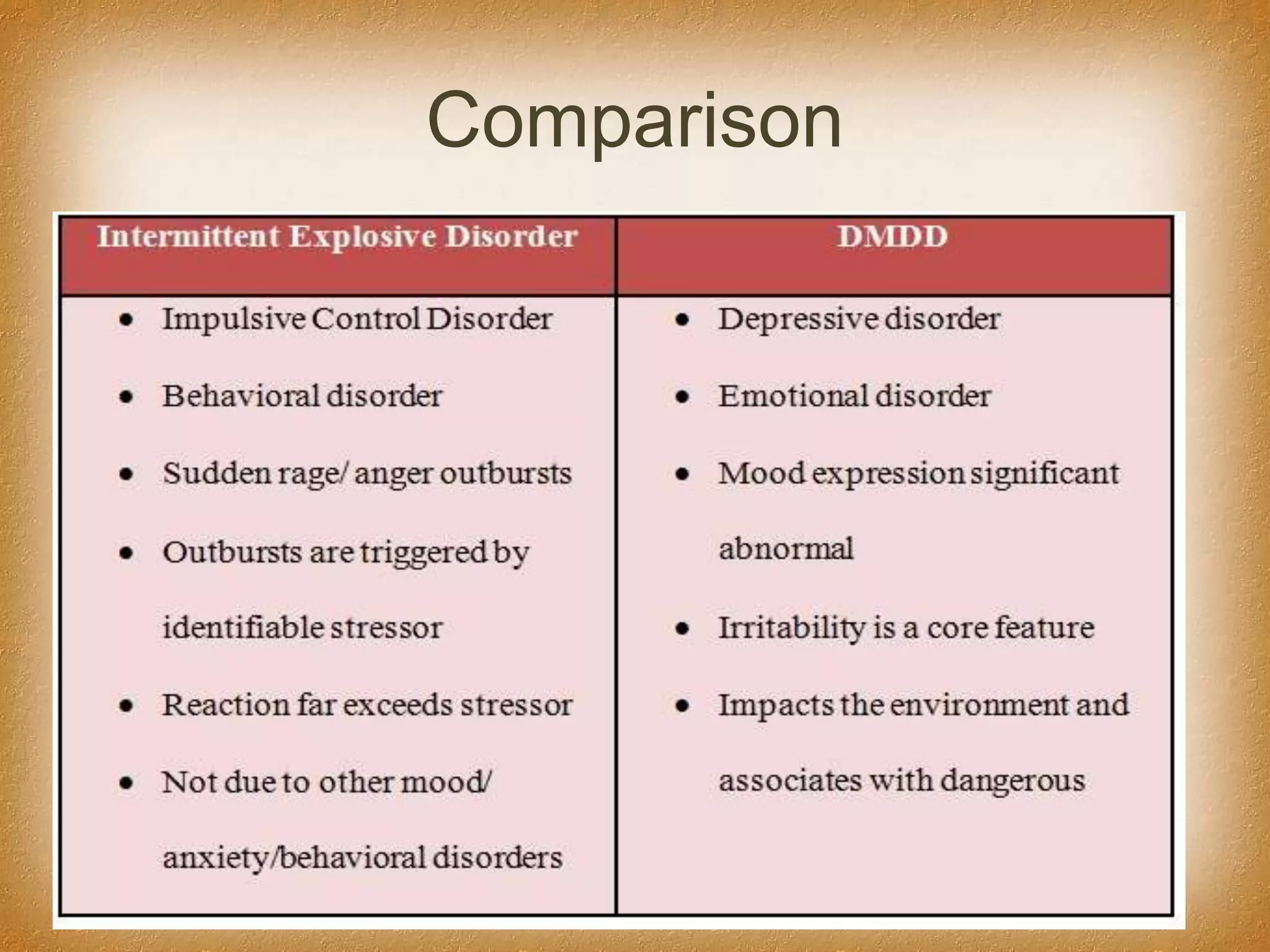
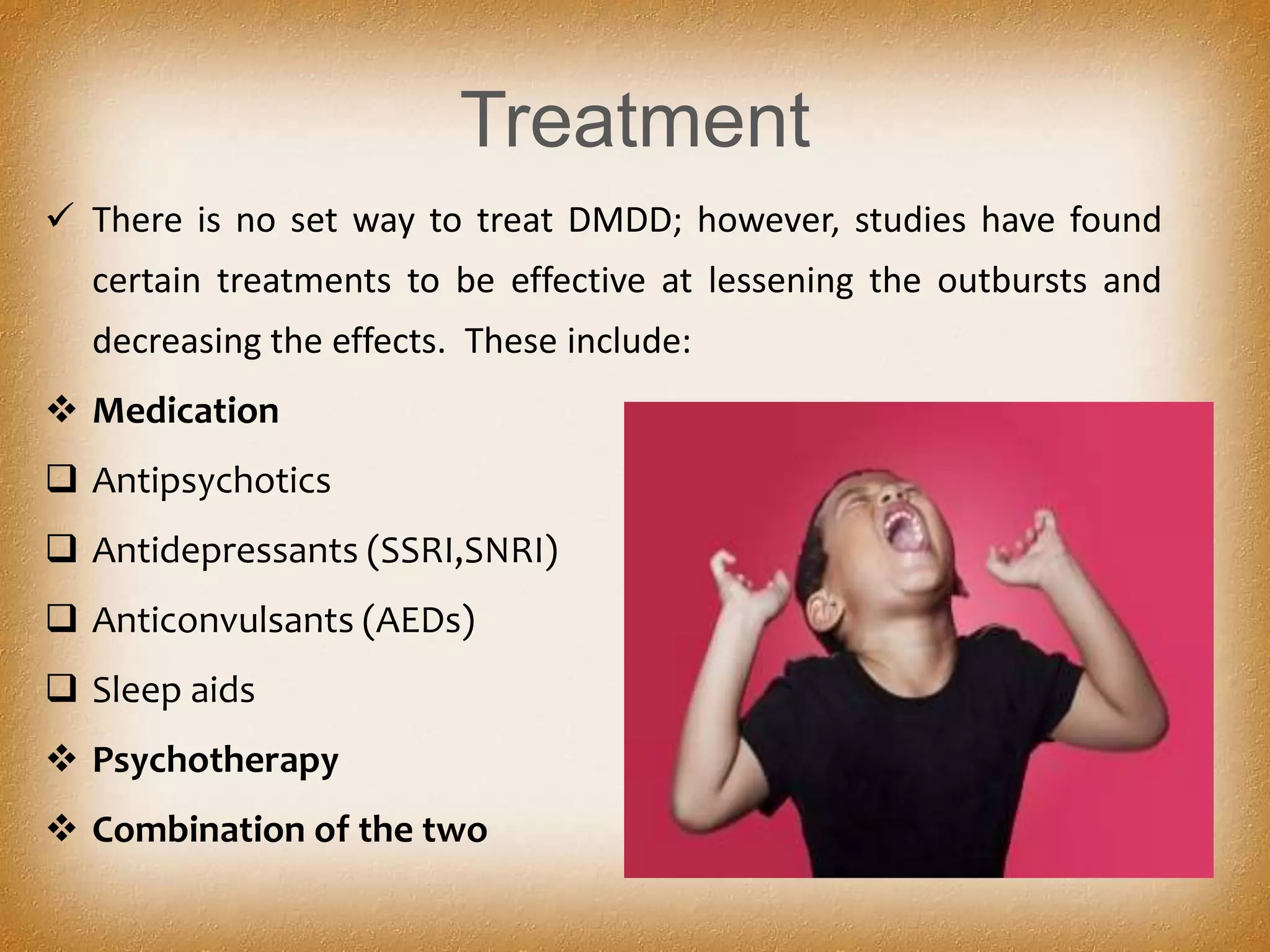
DMDD is a new diagnosis in the DSM-5 for children who experience frequent and severe temper outbursts that impair their daily functioning. It was created to more accurately diagnose children previously diagnosed with bipolar disorder. Children with DMDD experience chronic irritability and temper outbursts at least 3 times per week that are out of proportion to triggers. Treatment involves medication such as antidepressants and antipsychotics as well as psychotherapy. DMDD aims to reduce misdiagnosis of bipolar disorder in children and correctly identify those with severe irritability issues.












![DSM V Criteria
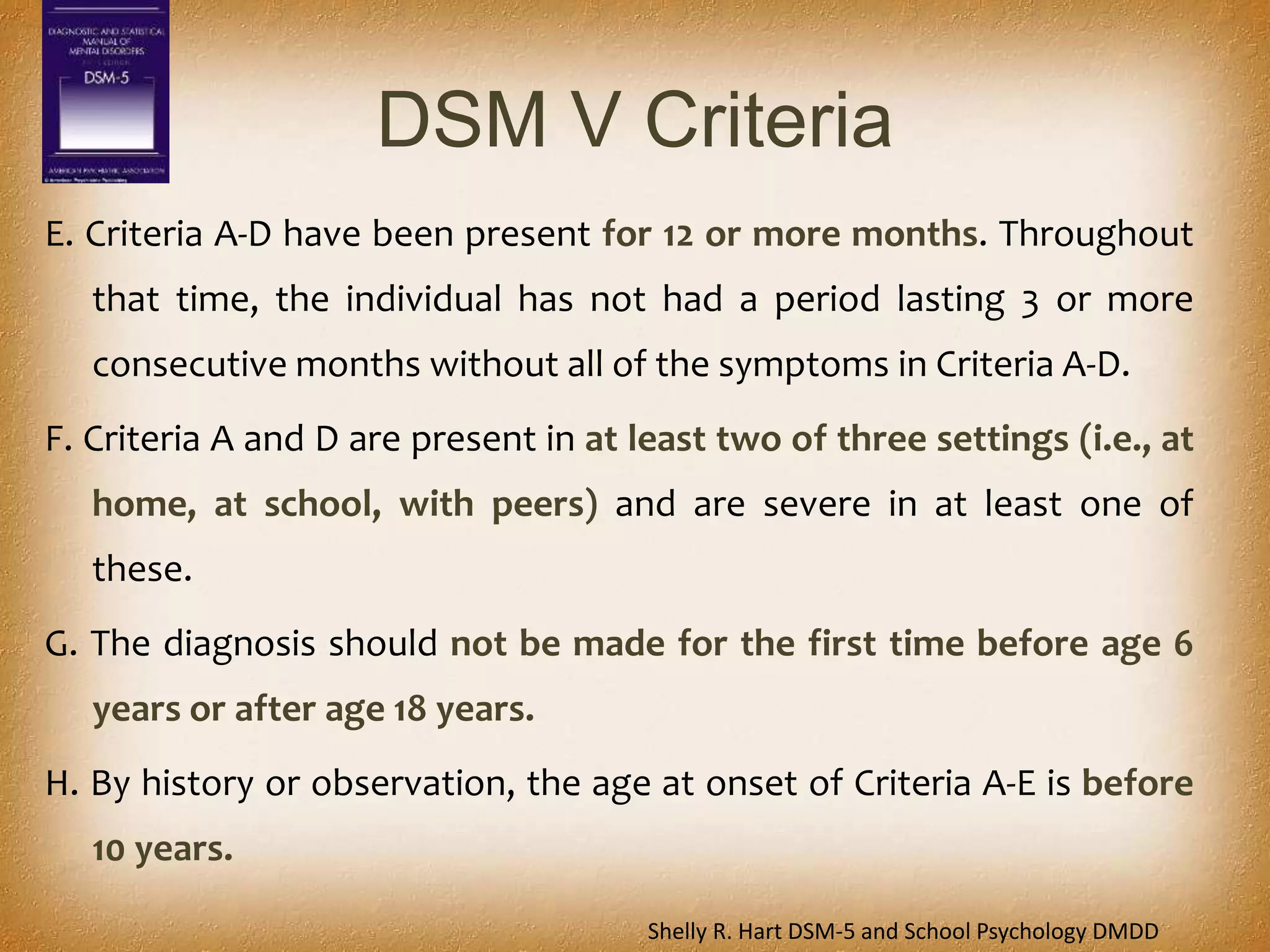
I. There has never been a distinct period lasting more than 1 day during
which the full symptom criteria, except duration, for a manic or
hypomanic episode have been met.
J. The behaviors do not occur exclusively during an episode of major
depressive disorder and are not better explained by another mental
disorder (e.g., autism spectrum disorder, posttraumatic stress
disorder, separation anxiety disorder, persistent depressive
disorder [dysthymia]).
K. The symptoms are not attributable to the physiological effects of a
substance or to an other medical or neurological condition
Shelly R. Hart DSM‐5 and School Psychology DMDD](https://image.slidesharecdn.com/dmdd-disruptivemooddysregulationdisorder-150511092655-lva1-app6892/75/Dmdd-disruptive-mood-dysregulation-disorder-15-2048.jpg)