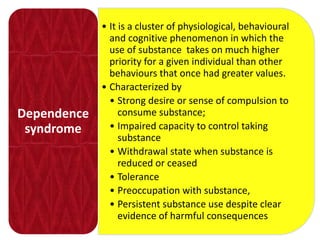
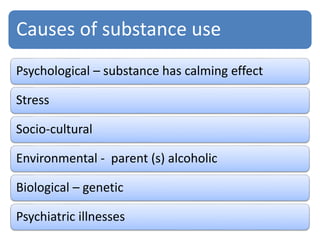
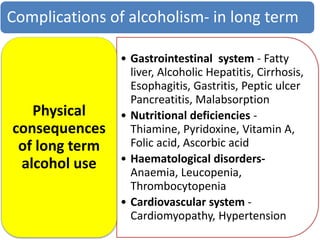
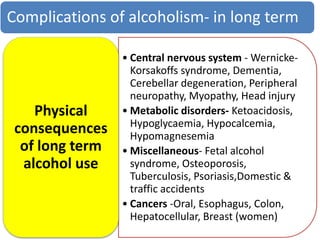
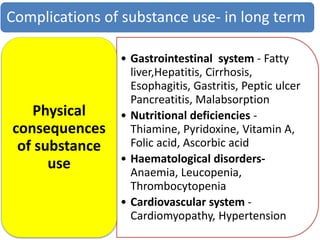
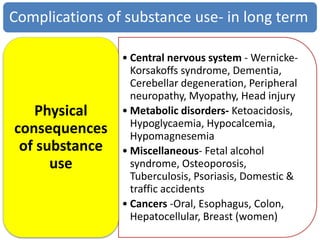
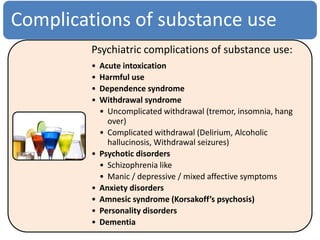
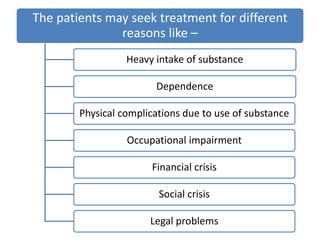
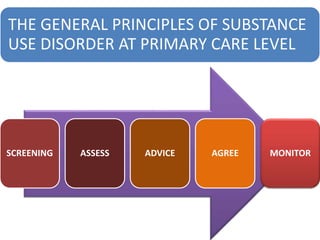
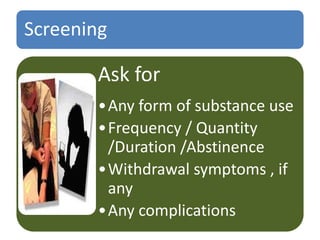
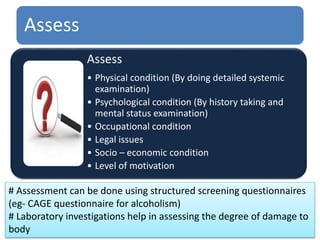
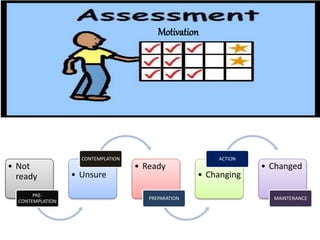
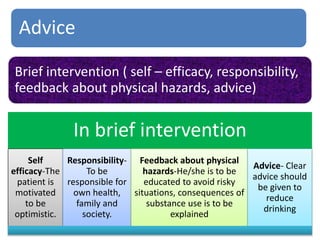
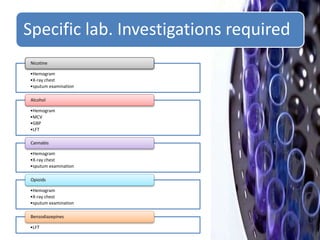
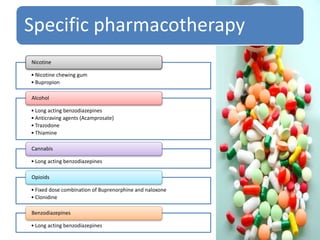
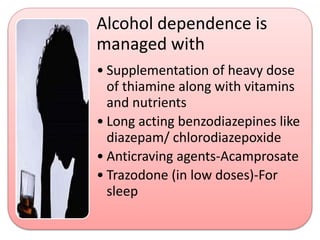
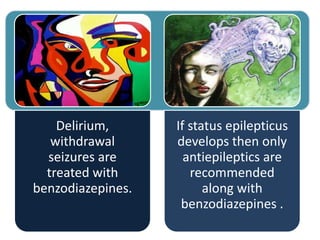
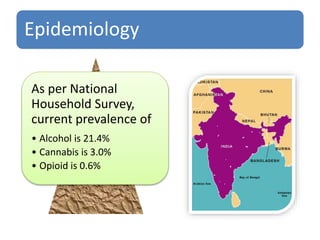
Substance use disorders are worldwide issues that affect people of all genders, races, and backgrounds. They are defined as a cluster of physiological and behavioral symptoms wherein substance use takes priority over other activities and responsibilities. Long term substance use can lead to both physical and psychological complications due to toxicity and dependence. Treatment involves screening, assessment, brief interventions, advice to quit, agreement to a treatment plan, pharmacotherapy tailored to the substance, and monitoring for withdrawal symptoms and continued abstinence. Non-pharmacological treatments like counseling are also important. Management at the primary care level can help address this widespread issue.


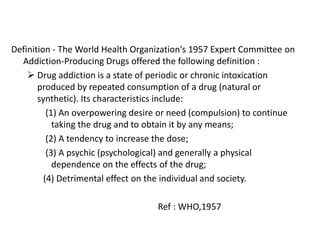
![The DSM, both in its revision of the third
edition (DSM–III–R; American Psychiatric
Association [APA] 1987) and in its most recent
edition (DSM– IV; APA 1994 and DSM-IV-TR;
2000), avoids the term addiction, preferring
instead to use the diagnoses of substance
abuse and dependence, collectively referred
to as substance use disorders.
Ref: APA: 1987, 1994, 2000](https://image.slidesharecdn.com/substanceusedisorder-171219150256/85/Substance-use-disorder-7-320.jpg)