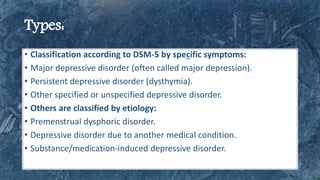
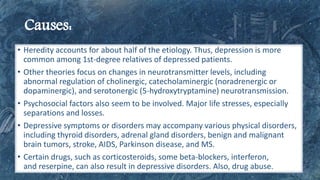
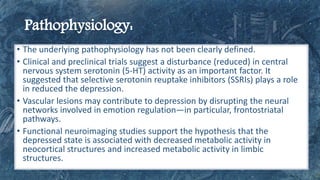
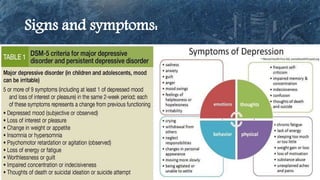
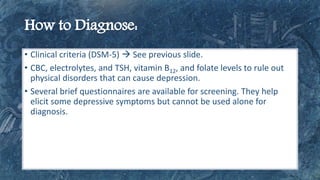
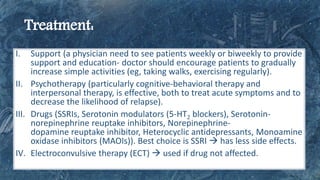
This document discusses depressive disorders, their classifications according to DSM-5, and contributing factors such as heredity and neurotransmitter changes. It highlights the importance of a comprehensive approach to treatment, including psychotherapy, medications, and support, to effectively manage symptoms and improve outcomes. Additionally, the document notes that while treatment can significantly reduce symptoms in many patients, some may not respond to initial treatments.