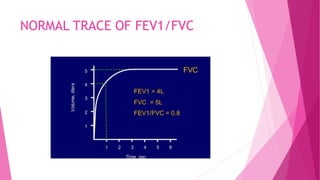
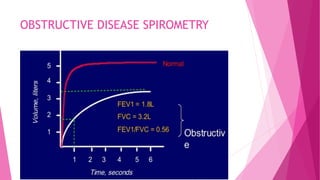
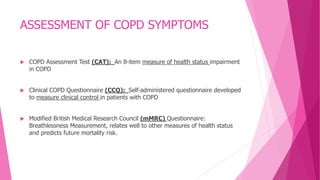
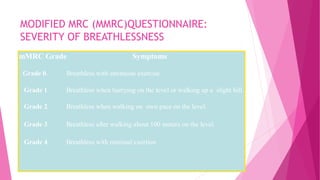
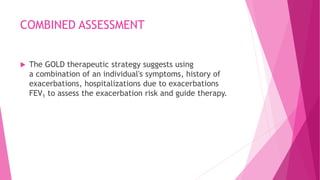
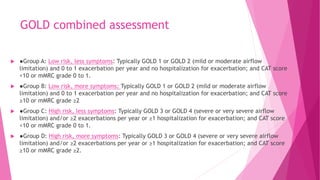
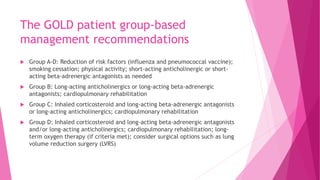
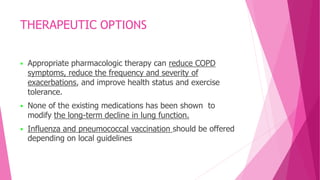
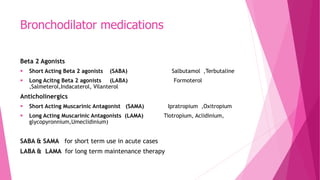
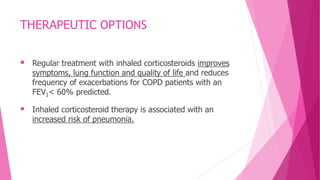
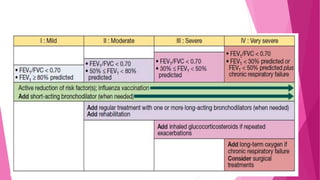
The document provides guidelines for grading and managing COPD according to GOLD guidelines. It discusses diagnosing COPD using spirometry and assessing severity based on symptoms, airflow limitation, and exacerbation risk. COPD is graded into 4 stages based on airflow limitation. Management is guided by combining assessments into Groups A through D, with Group D having the highest risk and most severe airflow limitation. Treatment options include smoking cessation, vaccination, bronchodilators, inhaled corticosteroids, oxygen therapy, and pulmonary rehabilitation.