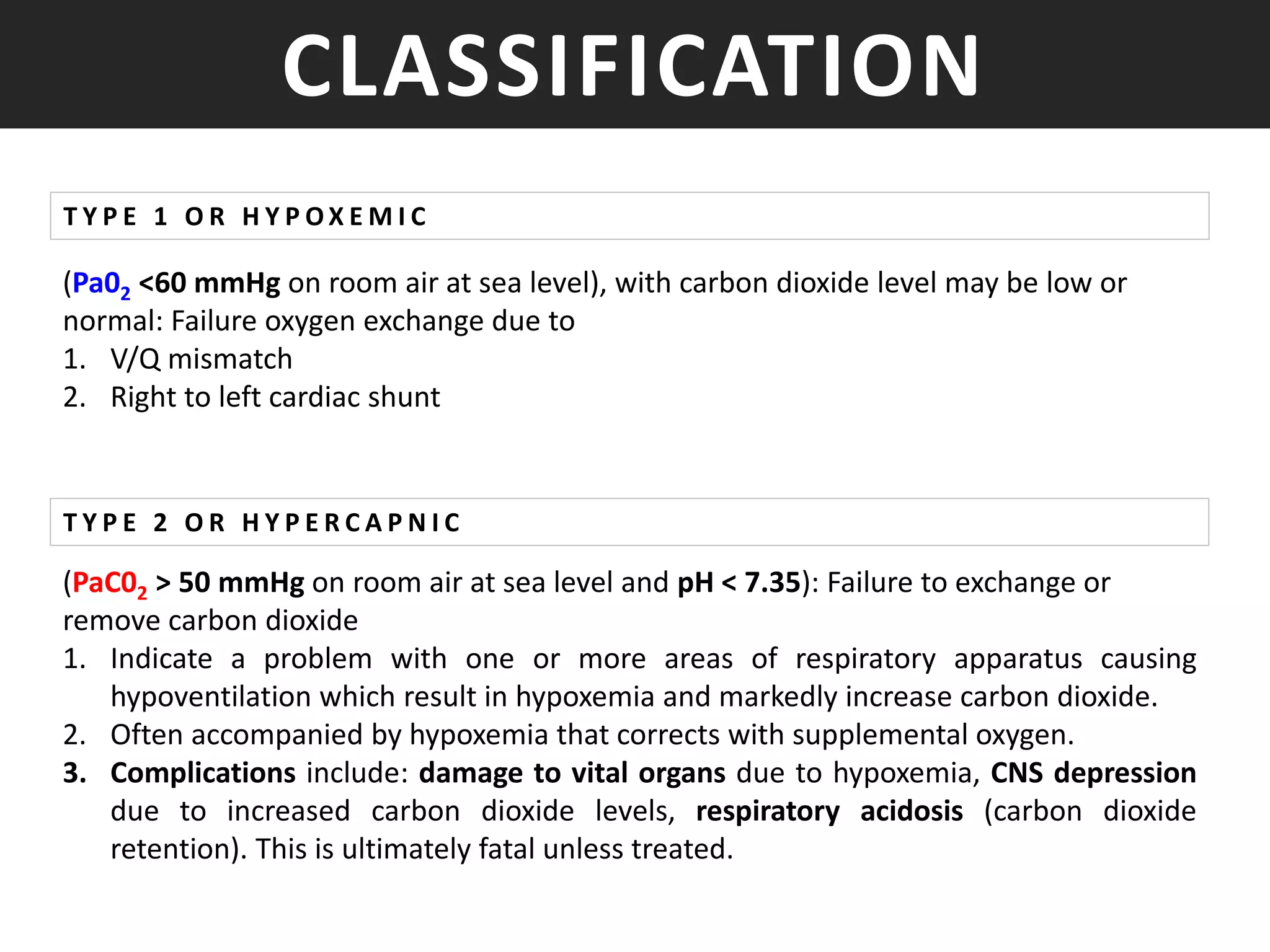
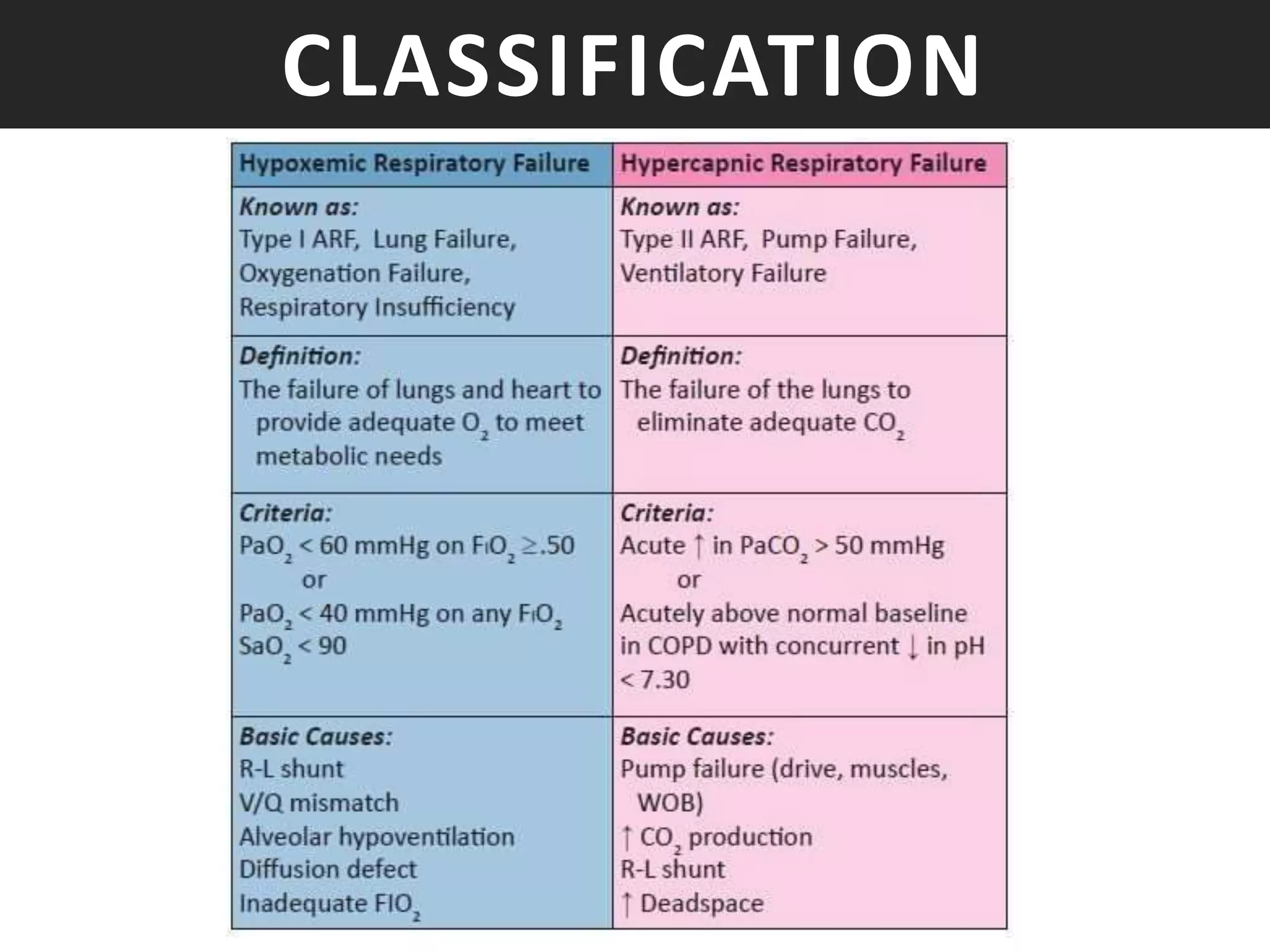
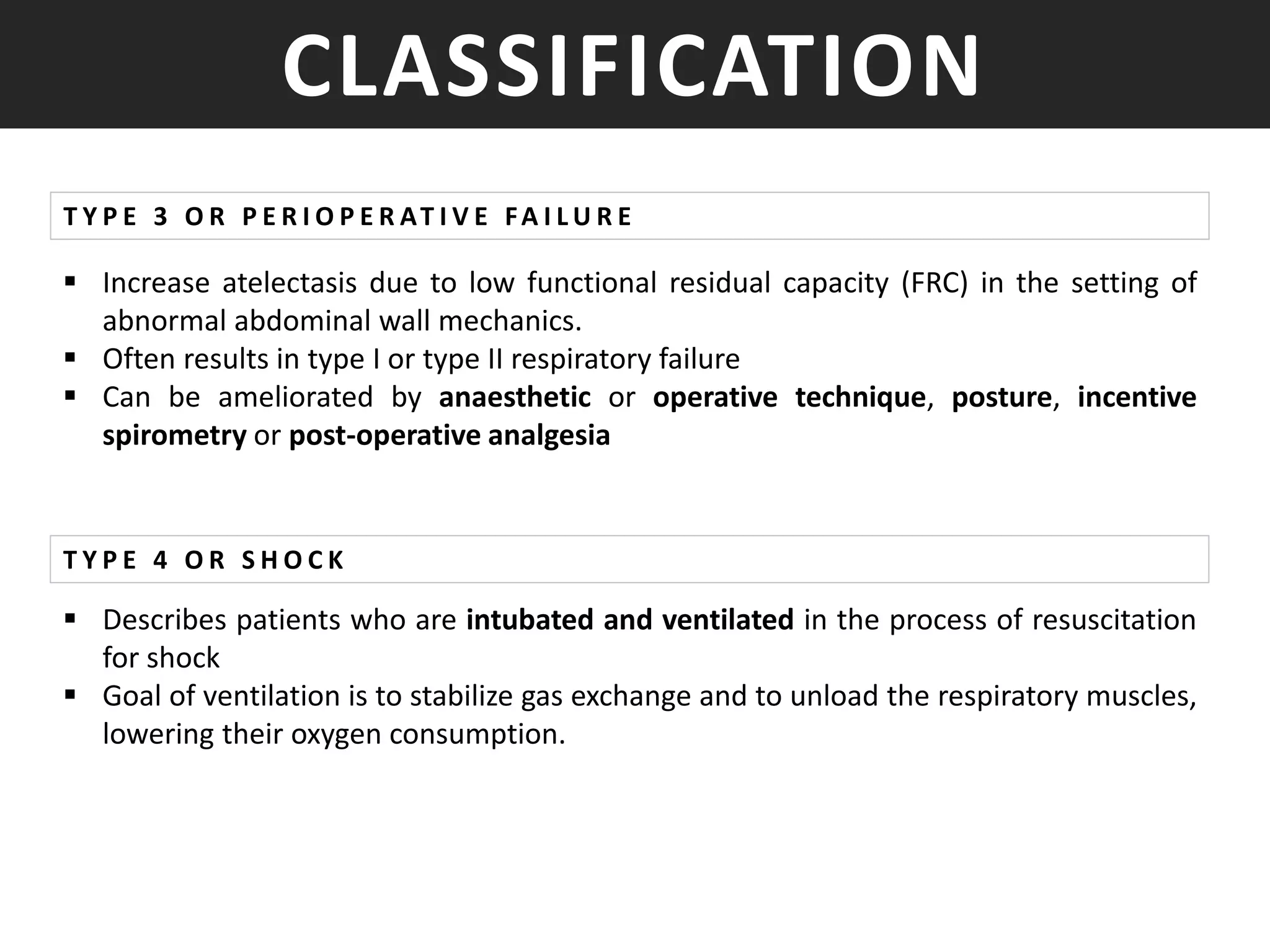
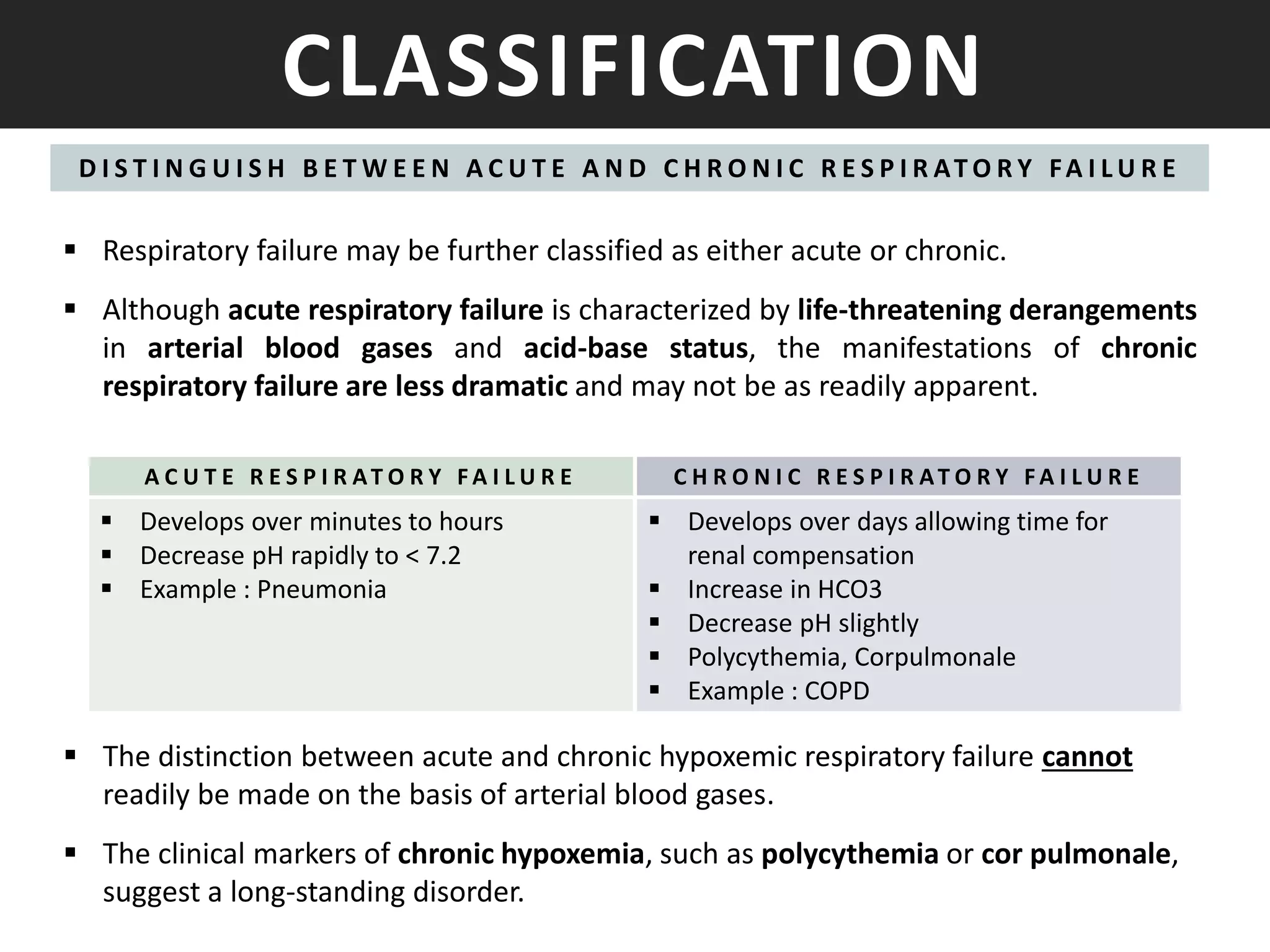
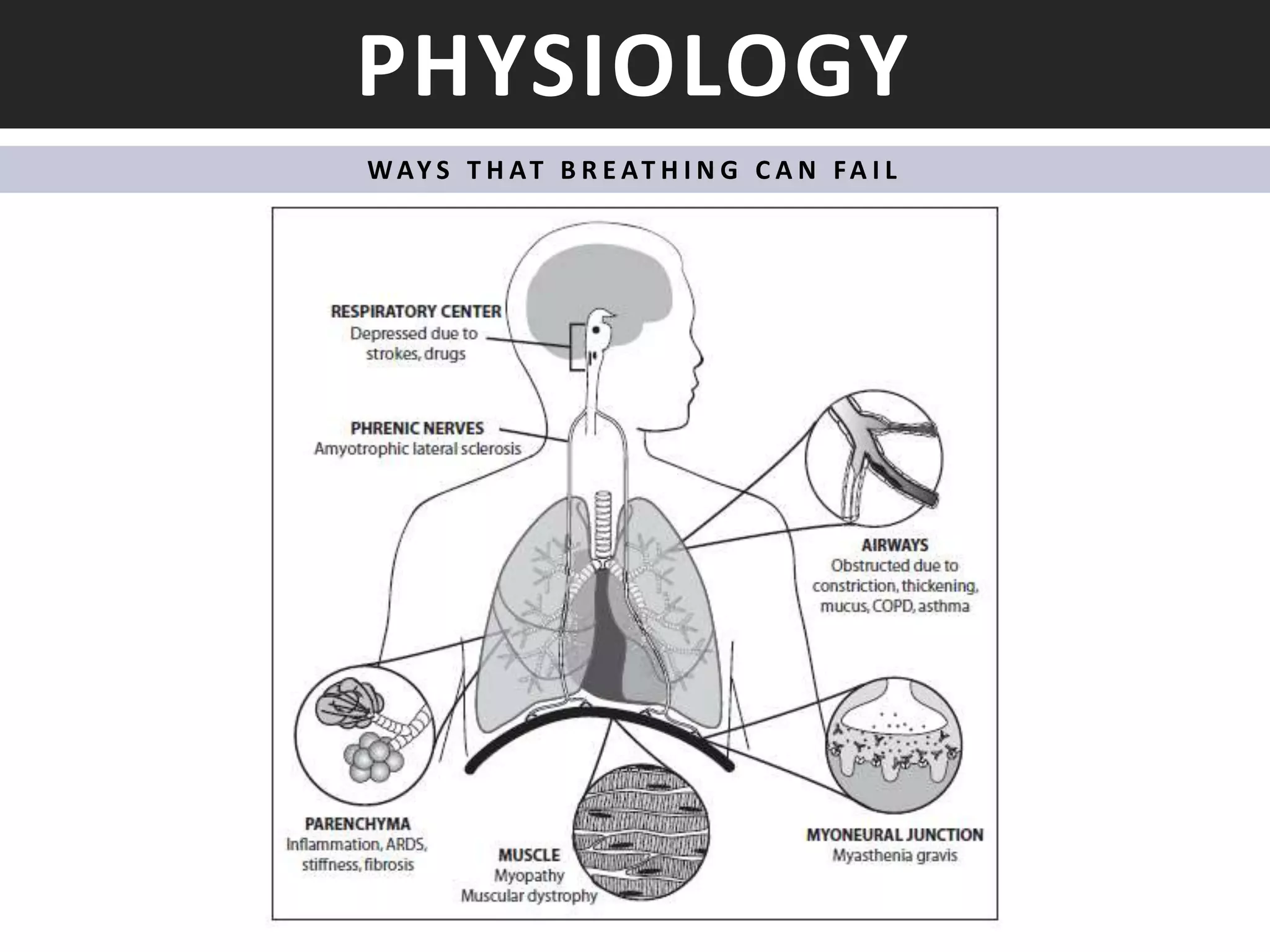
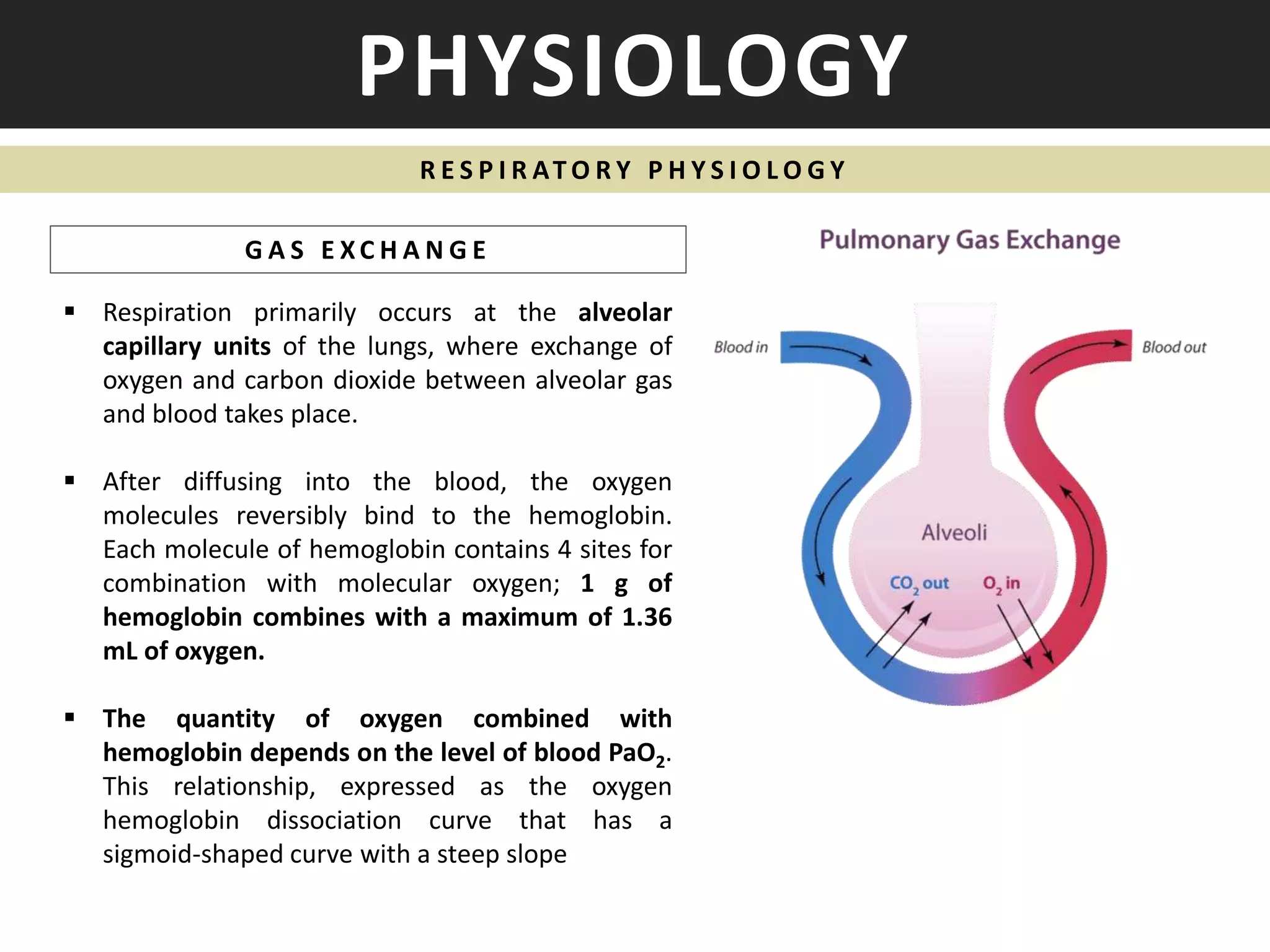
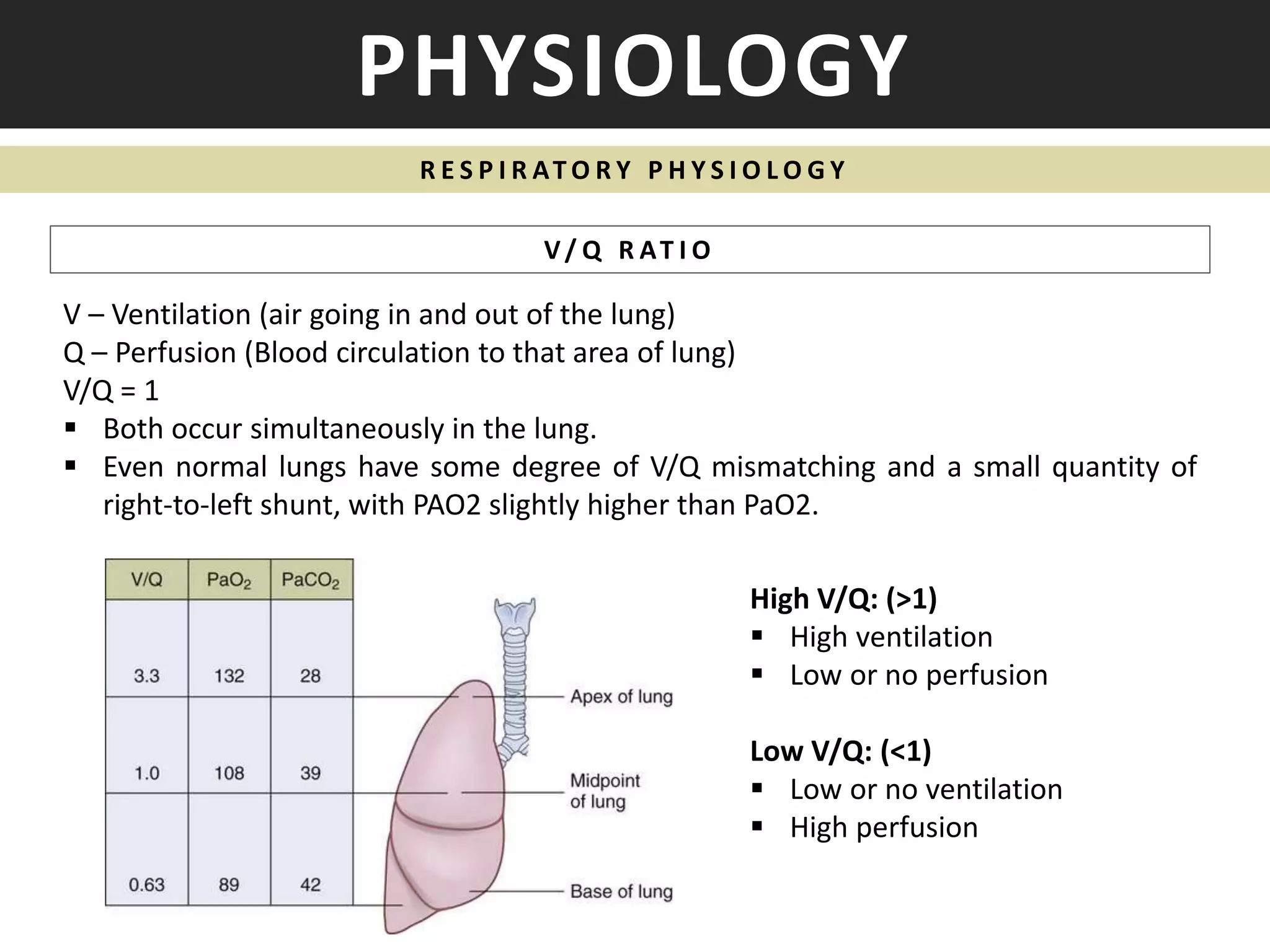
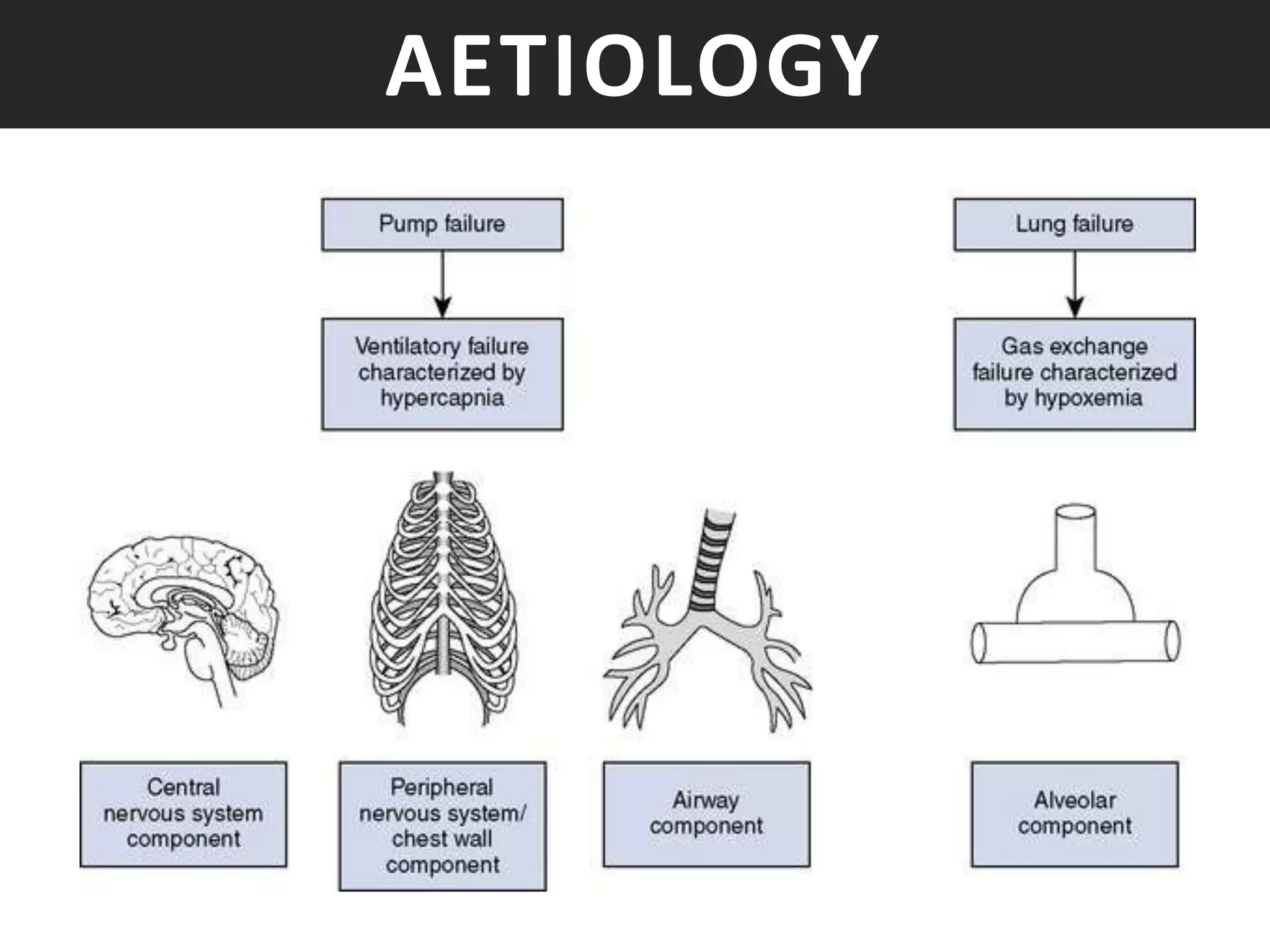
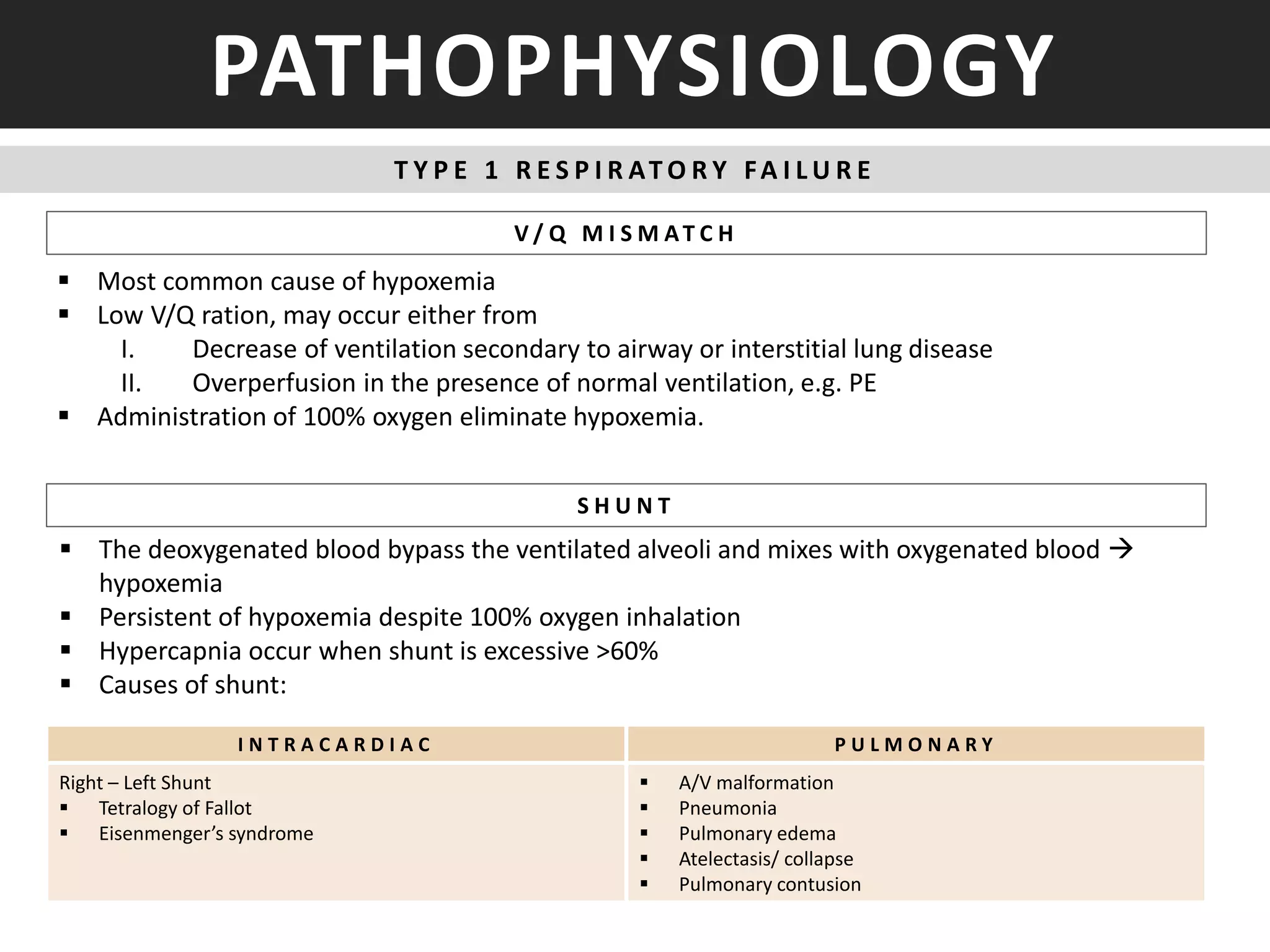
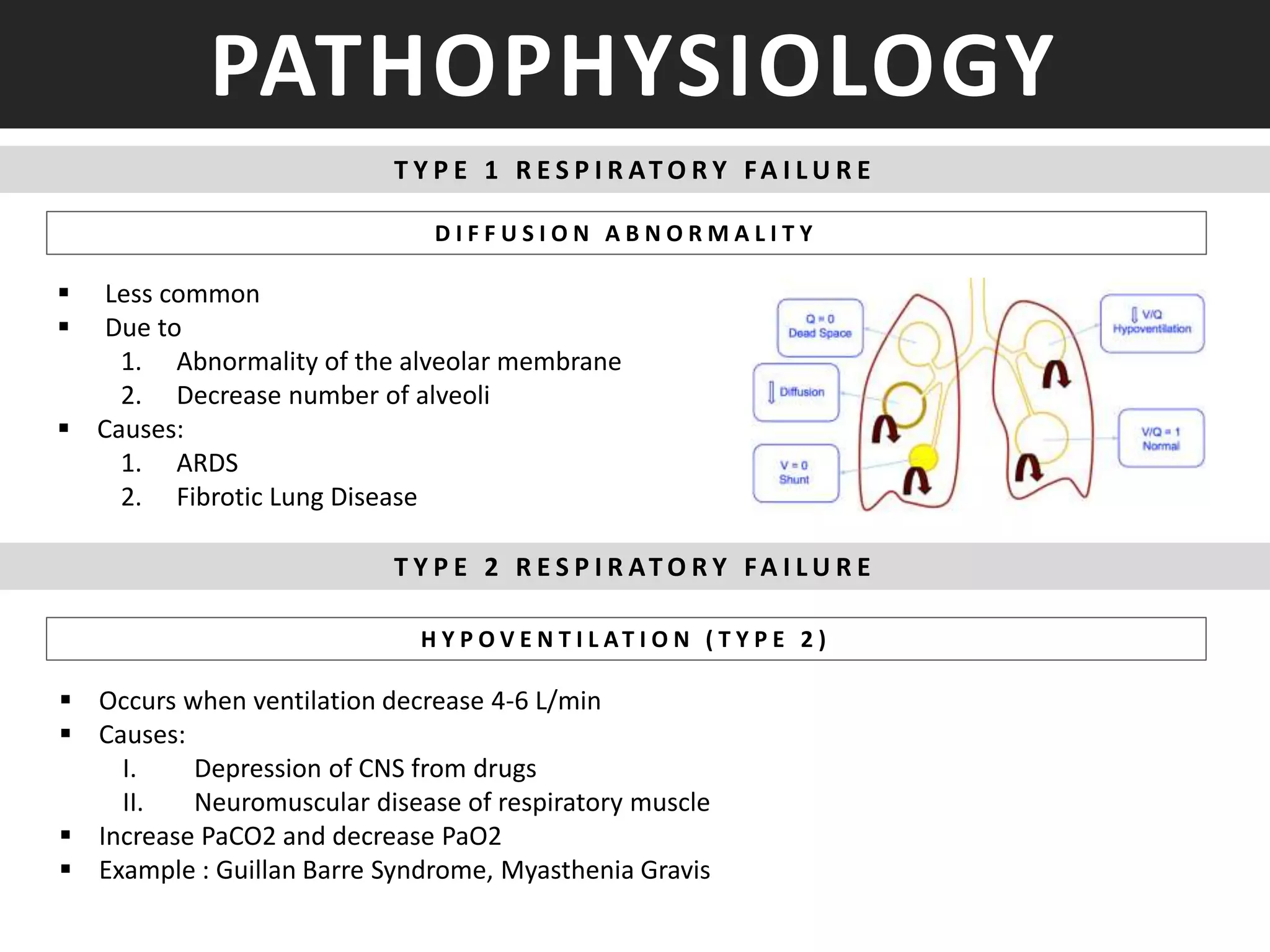
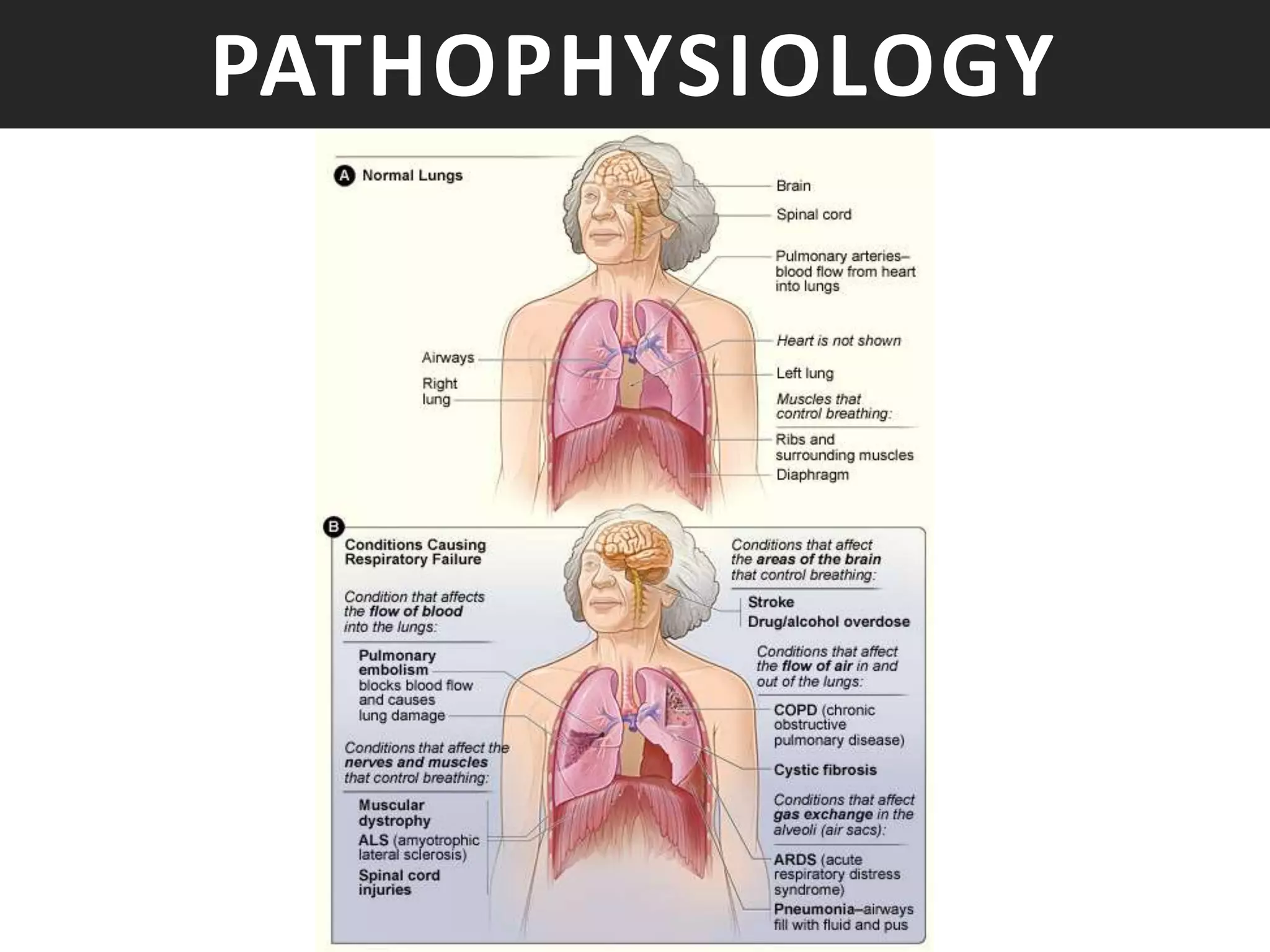
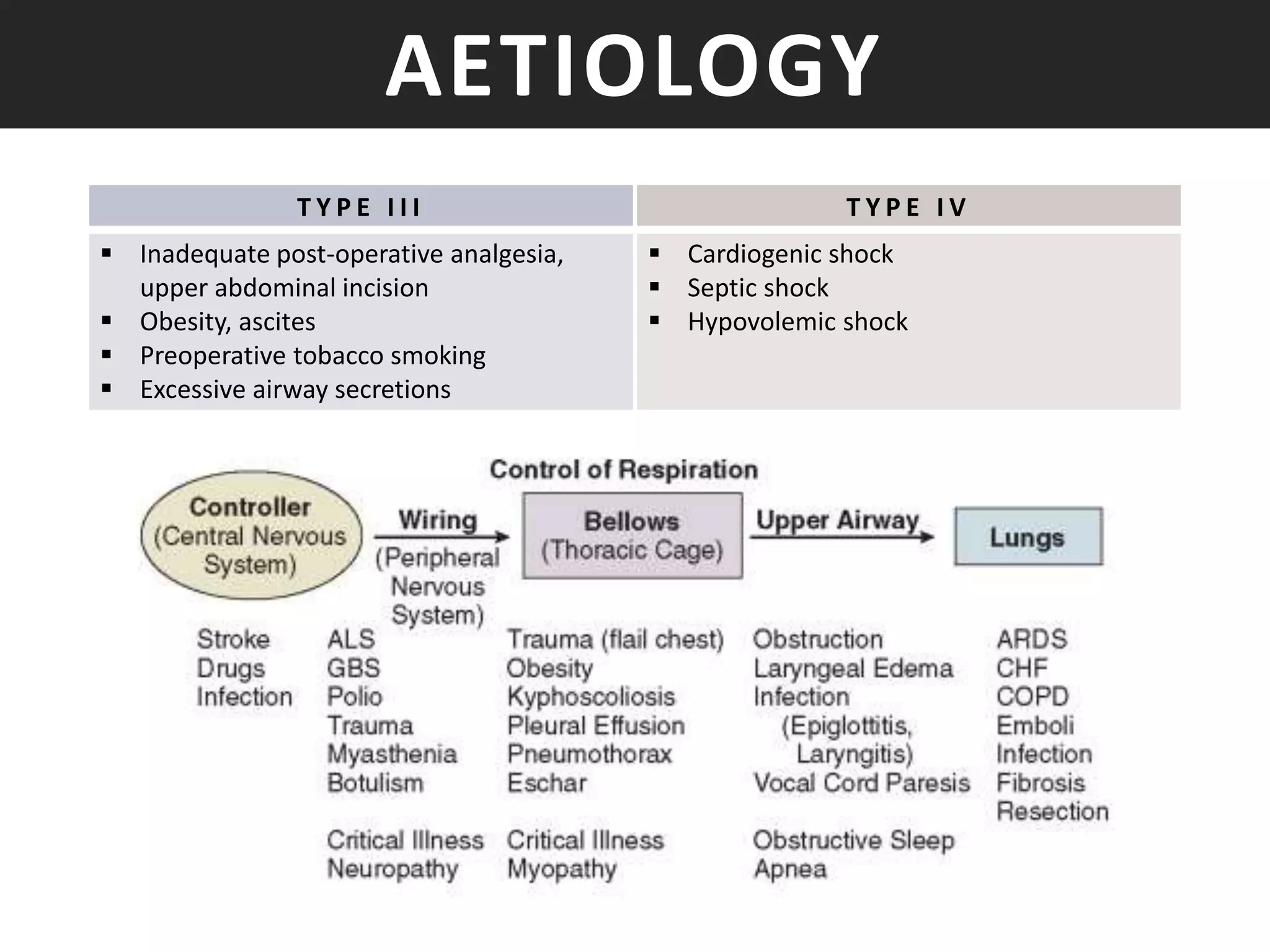
This document discusses respiratory failure, defined as inadequate oxygenation, ventilation, or both to meet metabolic demands. It can be classified as type 1 (hypoxemic) or type 2 (hypercapnic) respiratory failure. Risk factors include age, smoking, lung disease, and neurological or muscular disorders. Pathophysiology involves ventilation-perfusion mismatching, right-to-left shunting, or hypoventilation. Causes include pneumonia, pulmonary embolism, neuromuscular disorders, and acute respiratory distress syndrome. The control of breathing and gas exchange physiology are also summarized.