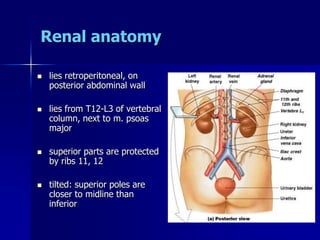
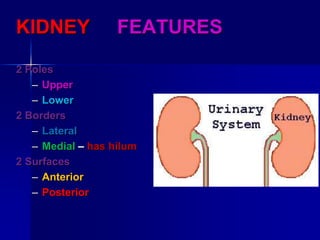
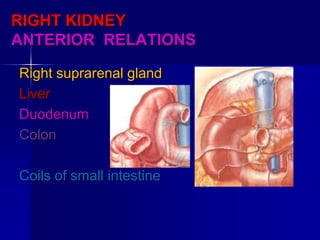
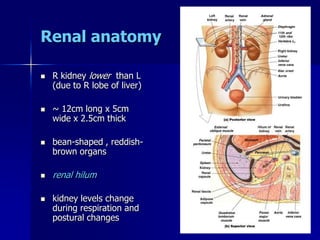
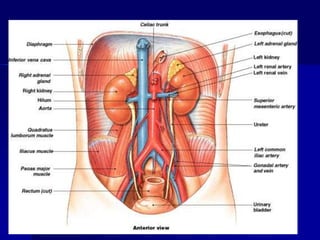
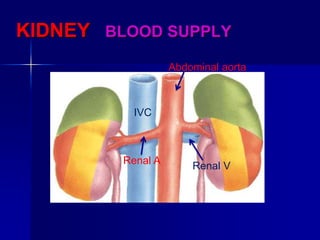
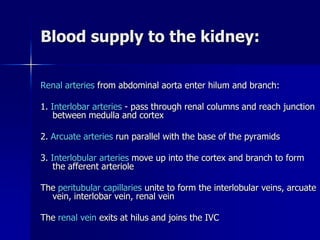
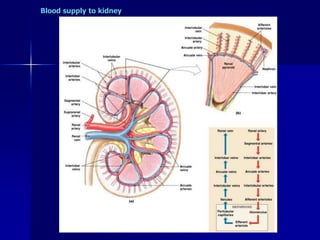
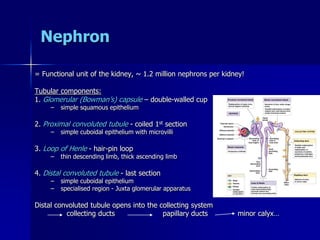
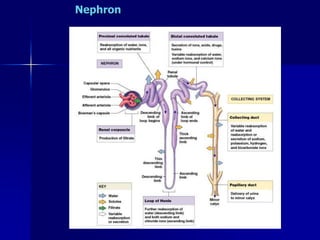
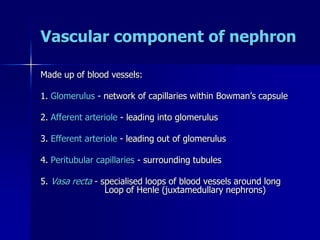
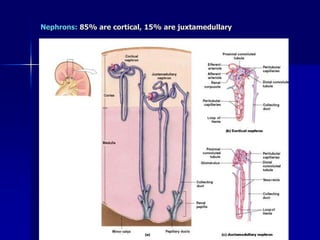
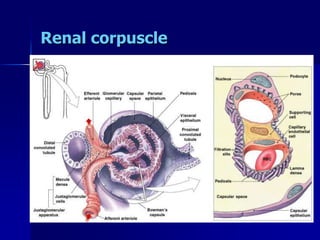
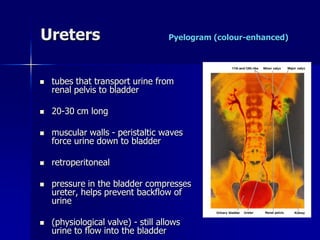
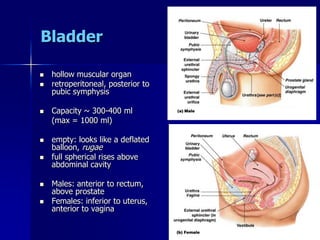
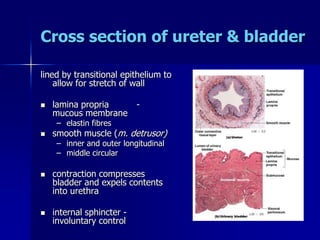
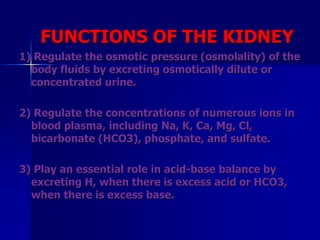
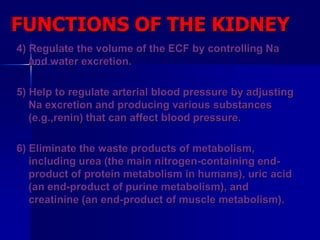
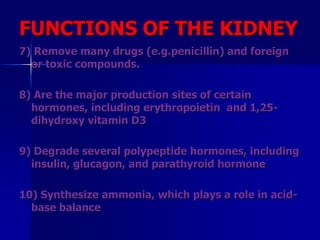
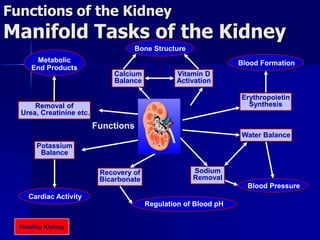
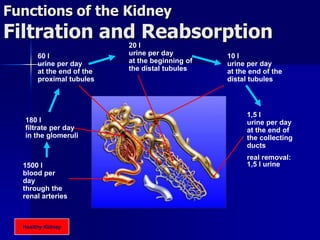
The document provides an overview of renal anatomy and physiology. It describes the key functions of the renal system as filtering waste from the blood and regulating fluid balance. The major structures include the kidneys, which filter blood and produce urine, the ureters which transport urine from the kidneys to the bladder, and the bladder which acts as a reservoir for urine storage. The kidneys contain nephrons, which are the functional filtering units. Blood enters the nephrons via the renal arteries and is filtered in the glomerulus. Urine is produced and drains through the renal tubules and collecting duct system.