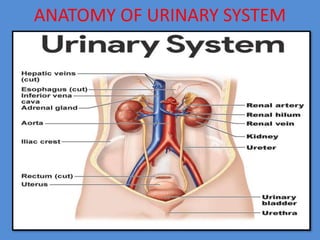
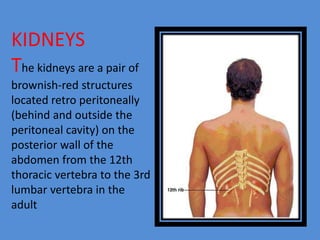
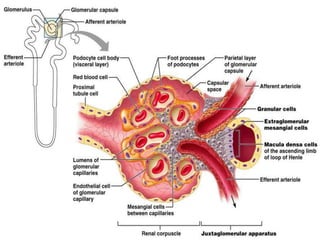
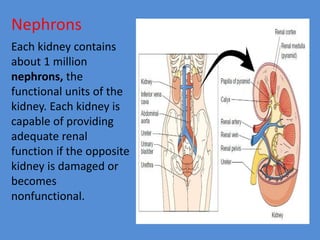
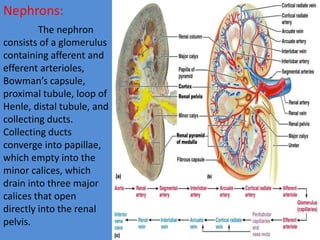
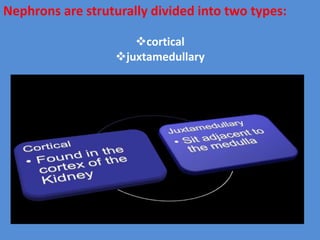
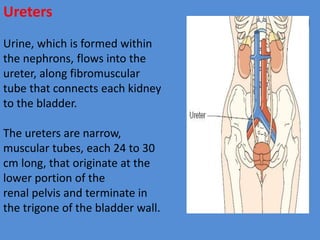
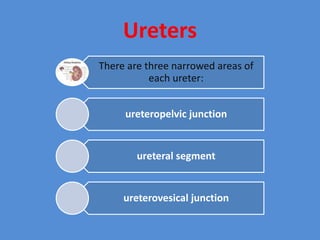
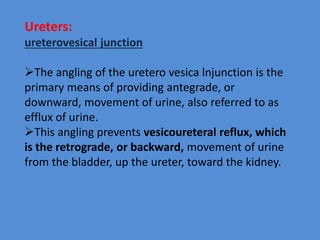
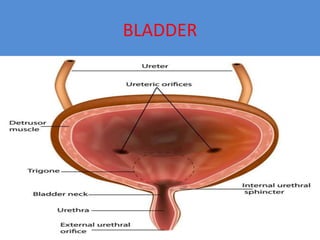
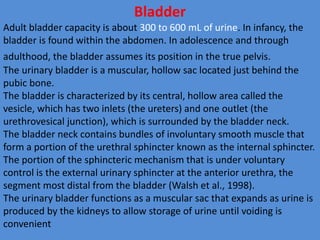
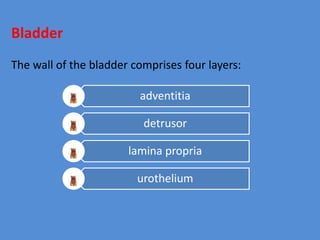
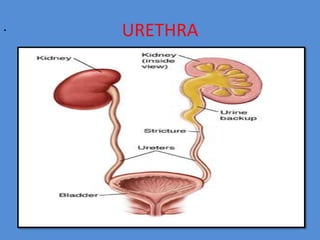
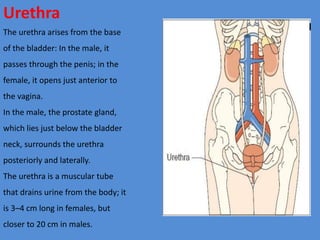
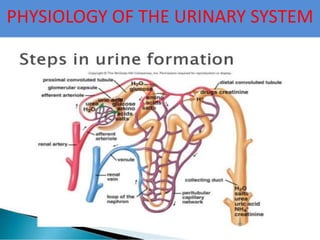
The document describes the anatomy and physiology of the urinary system. It details the major structures including the kidneys, ureters, bladder, and urethra. It explains that the kidneys filter waste from the blood to produce urine and regulate important processes in the body. Urine travels from the kidneys through the ureters to the bladder, then exits through the urethra. Key functions of the urinary system include waste excretion, fluid and electrolyte balance, and blood pressure regulation.