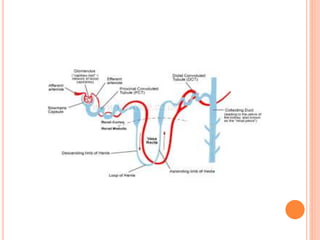
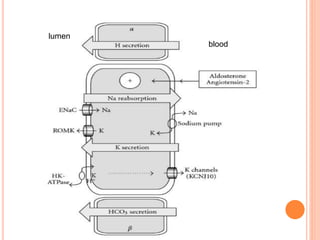
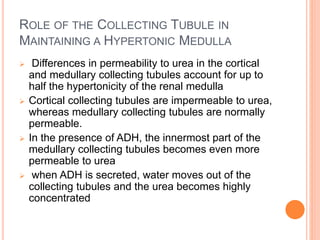
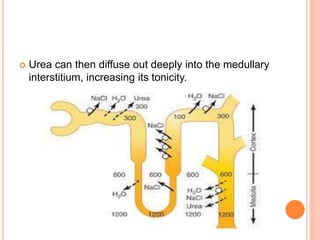
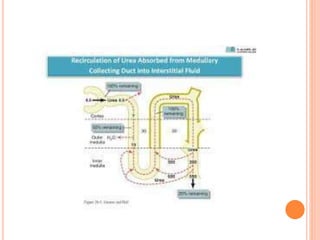
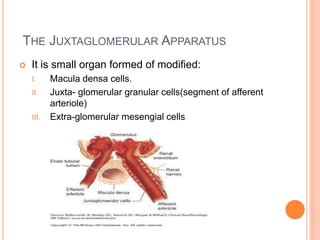
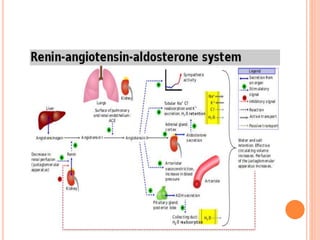
This document summarizes the anatomy and physiology of the nephron, specifically the collecting tubules and juxtaglomerular apparatus. The collecting tubule is the final segment of the nephron before entering the collecting duct system. It can be divided into the cortical and medullary collecting tubules. The cortical collecting tubule reabsorbs sodium, potassium, and water. The medullary collecting tubule is responsible for acidification of urine and is permeable to water and urea. The juxtaglomerular apparatus is formed by modified cells in the afferent arteriole and macula densa. It detects changes in chloride concentration and blood pressure, triggering the release of renin and regulating the