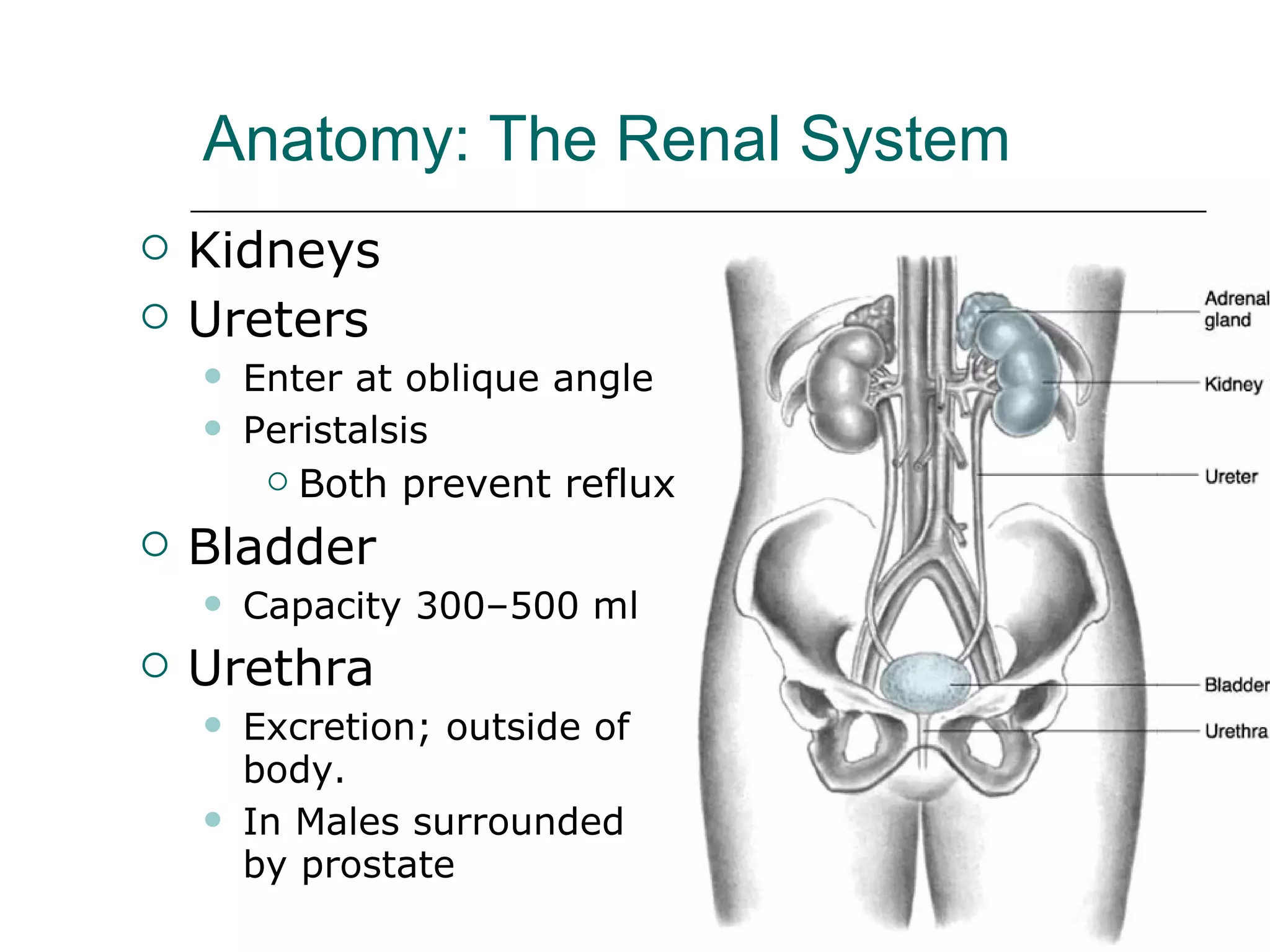
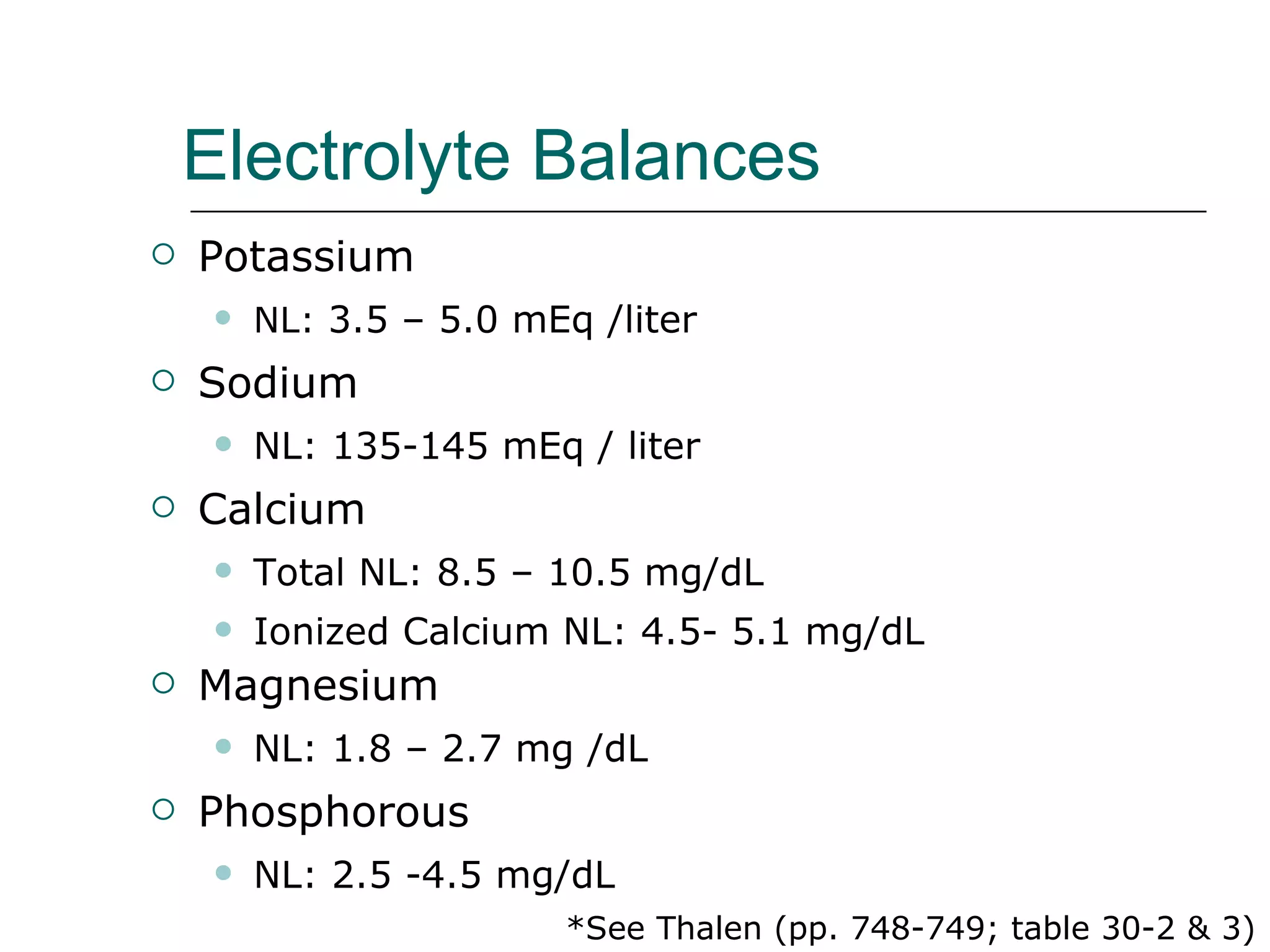
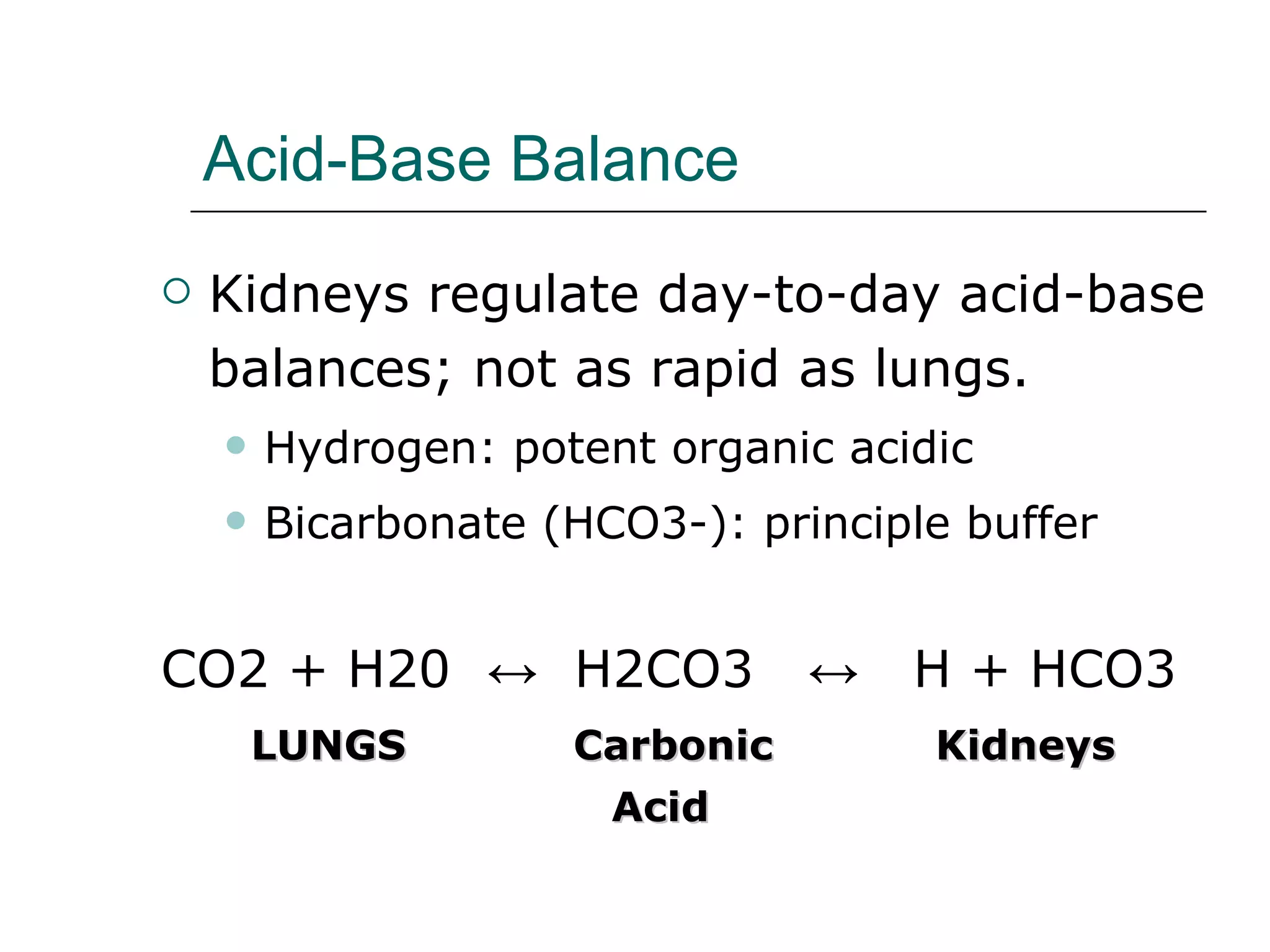
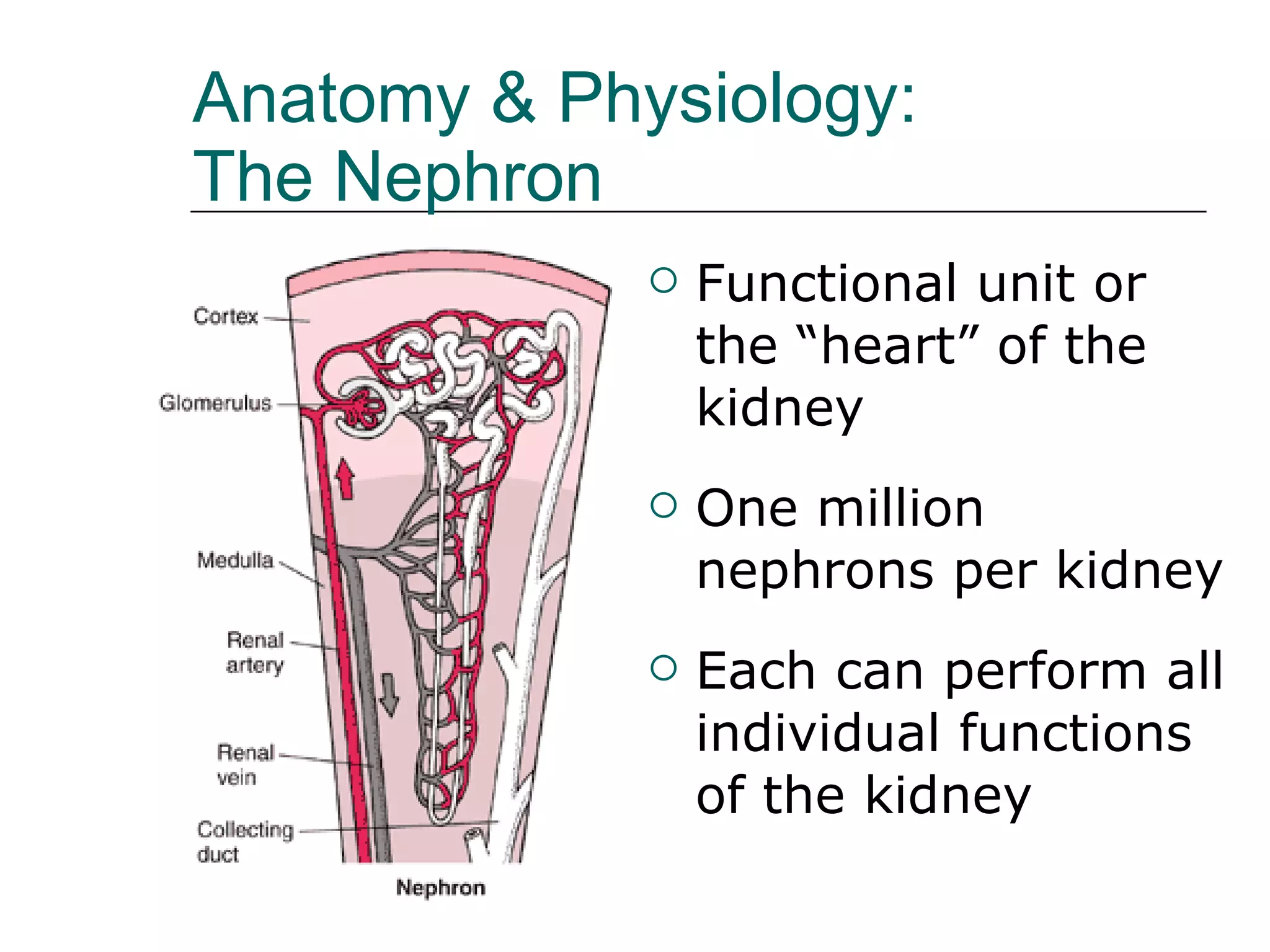
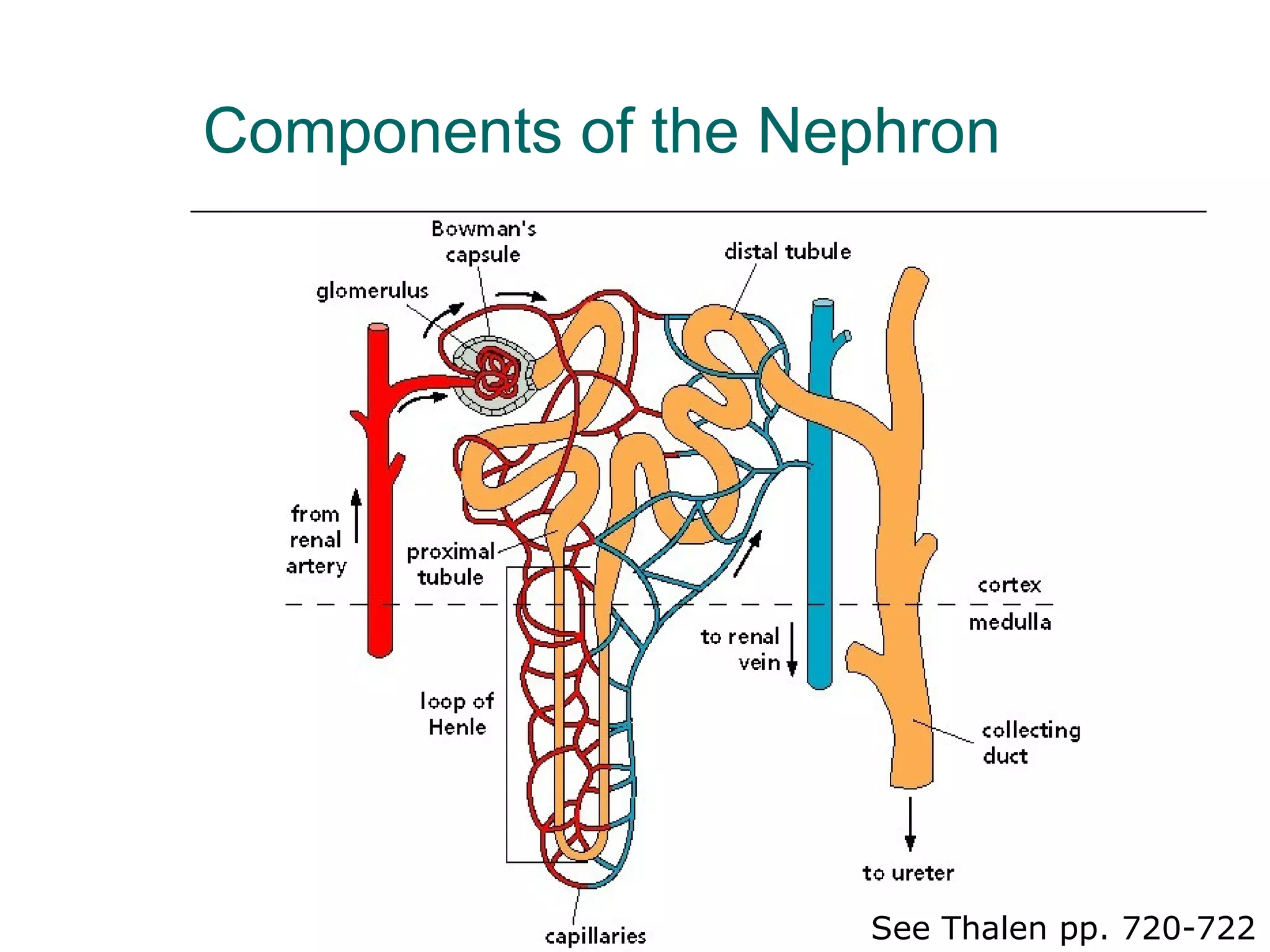
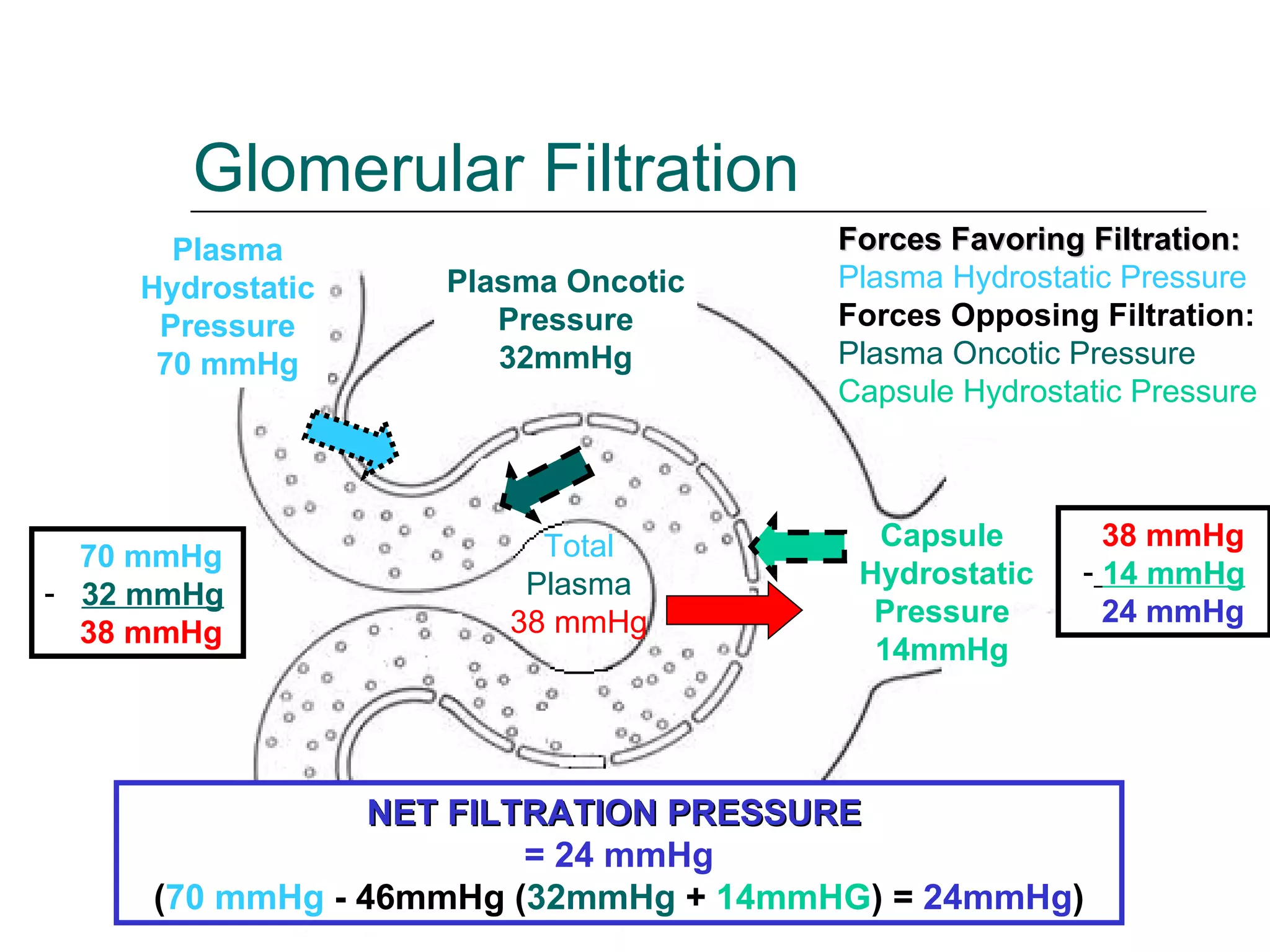
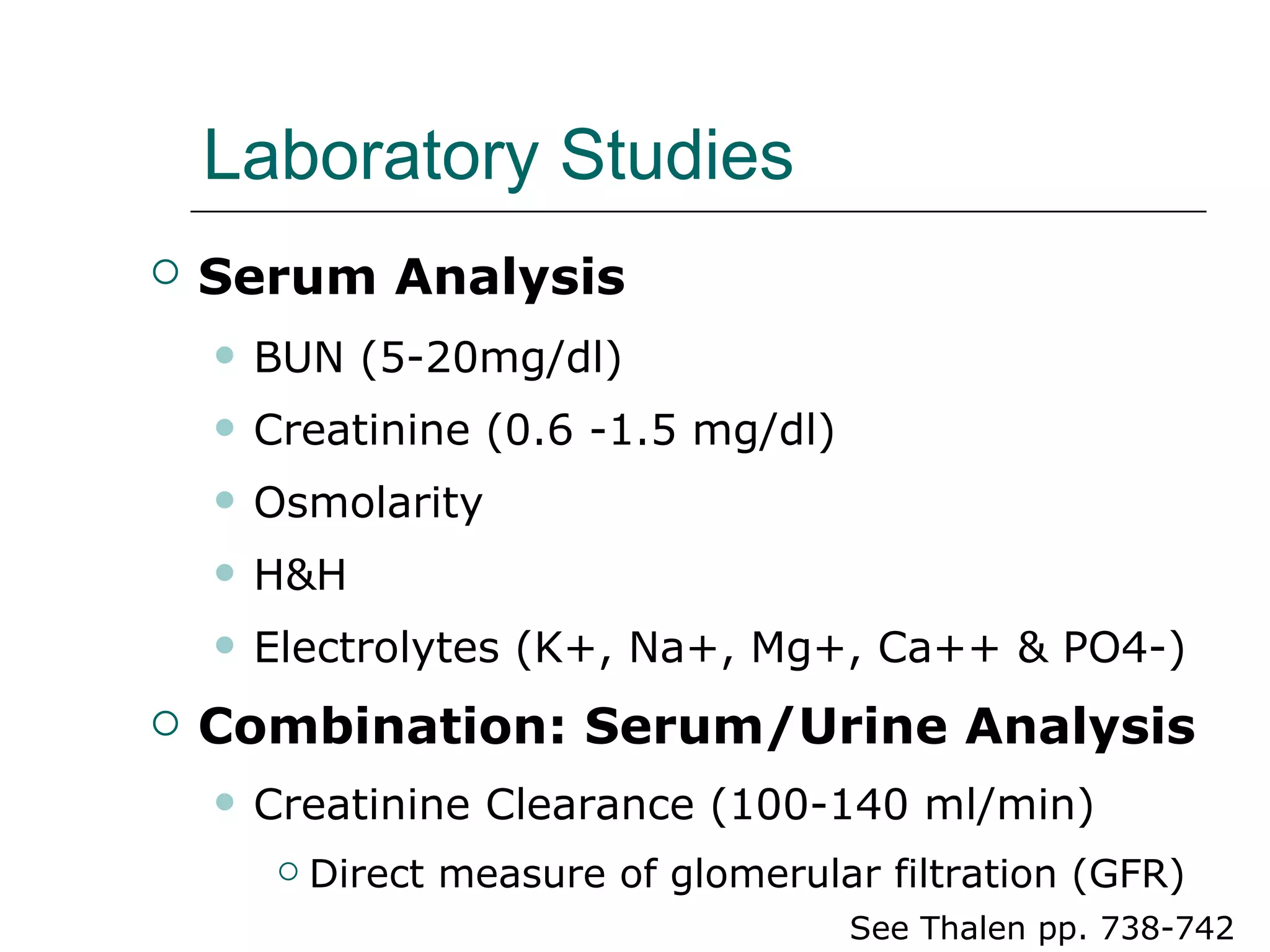
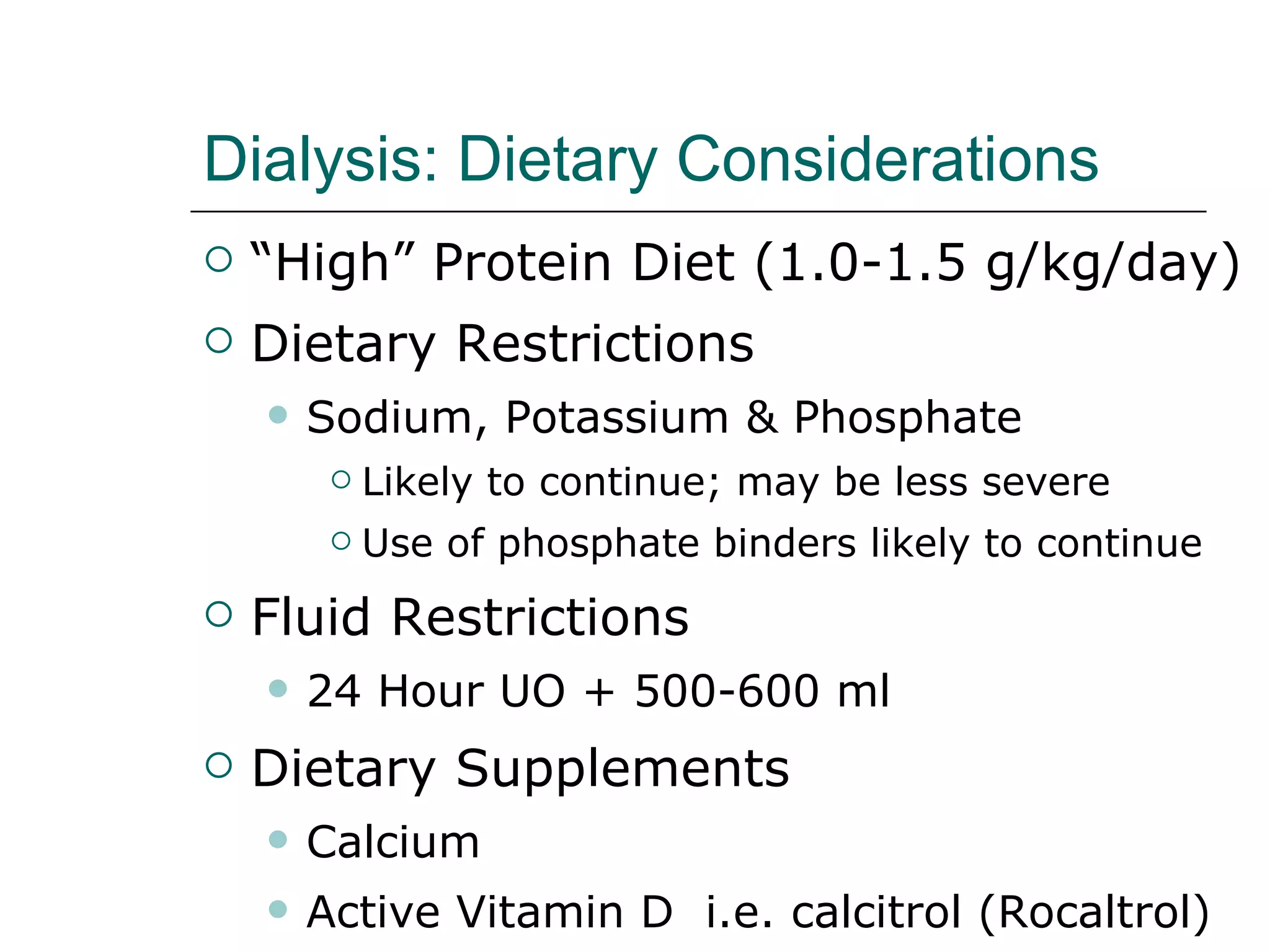
The renal system consists of the kidneys, ureters, bladder and urethra. The kidneys filter waste from the blood and regulate electrolytes and fluid balance. They produce erythropoietin to stimulate red blood cell production and activate vitamin D to regulate calcium levels. Renal failure occurs when kidney function declines, leading to the buildup of waste and imbalances in fluid, electrolytes and acid-base levels. Treatment options for renal failure include dialysis and transplantation.