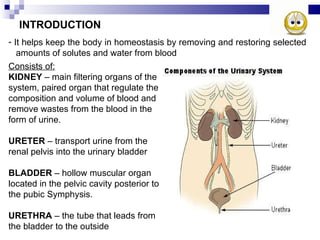
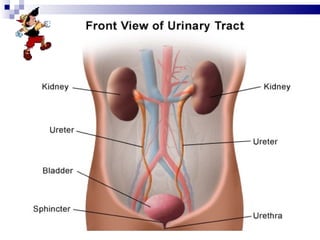
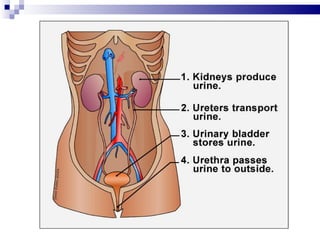
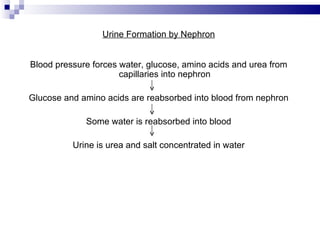
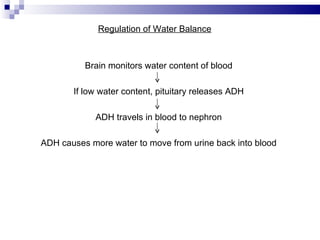
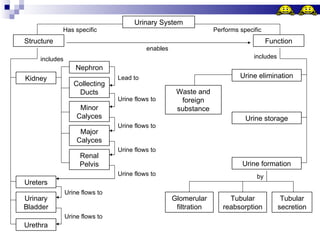
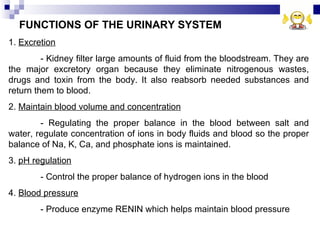
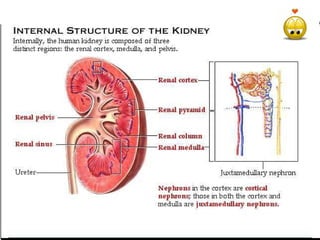
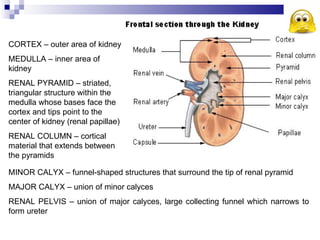
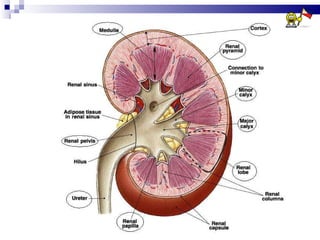
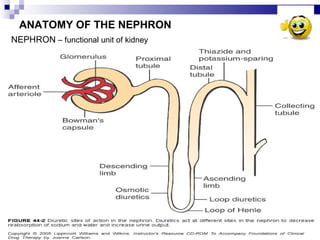
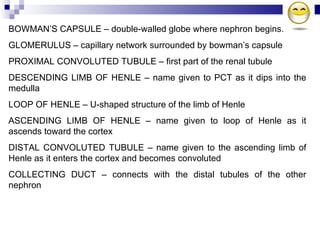
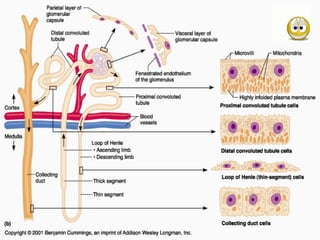
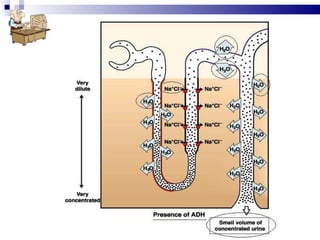
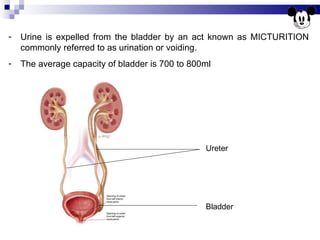
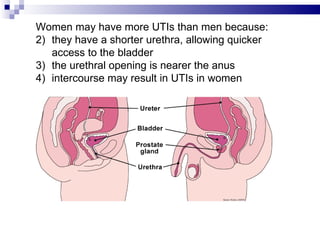
The urinary system consists of the kidneys, ureters, bladder and urethra. The kidneys filter waste from the blood to produce urine. The nephrons in the kidneys remove wastes and regulate water and electrolyte balance. Urine travels from the kidneys down the ureters to the bladder. When full, the bladder contracts to expel urine through the urethra. The system helps maintain homeostasis by regulating water balance and removing toxins from the body.