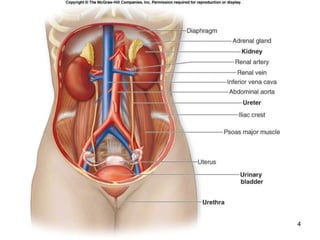
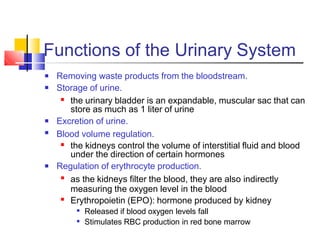
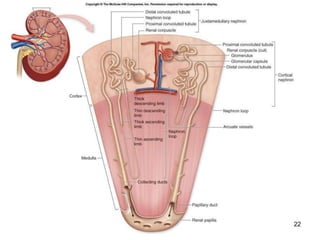
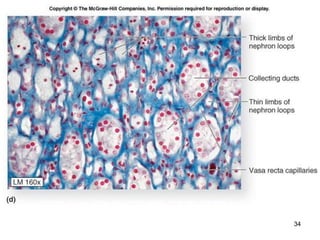
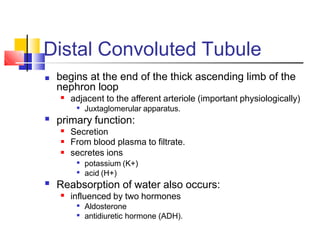
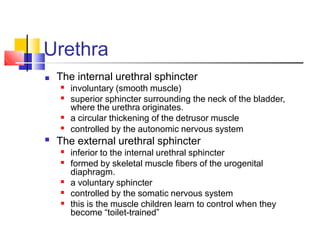
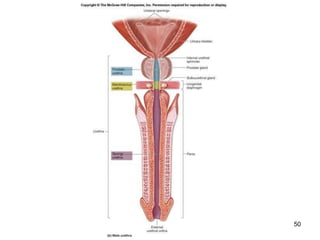
The urinary system removes waste from the bloodstream through the kidneys, which filter the blood to form urine. The urine passes from the kidneys to the bladder through ureters. The bladder stores urine until urination, when urine exits the body through the urethra. The kidneys contain nephrons, which filter blood in the glomerulus and remove waste from the filtrate through reabsorption and secretion as urine is formed.