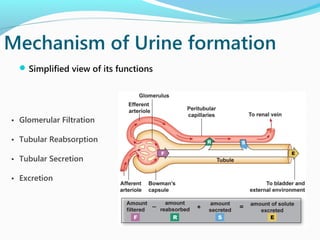
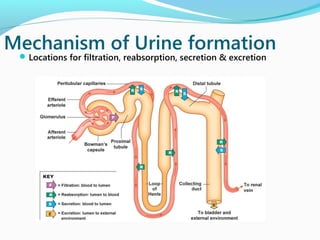
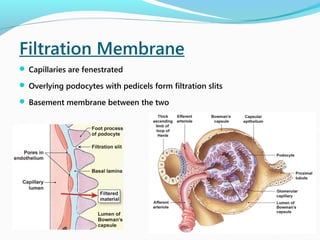
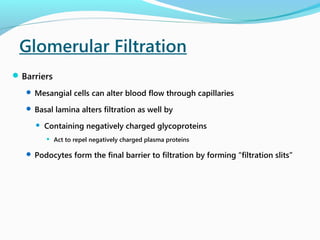
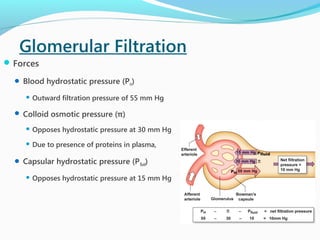
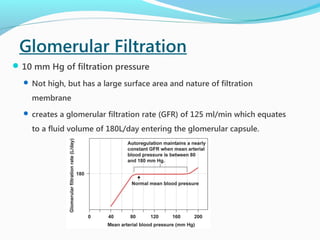
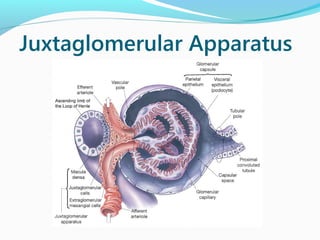
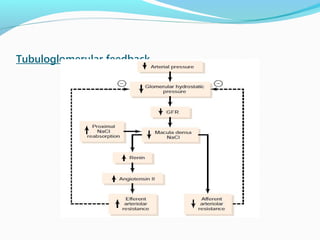
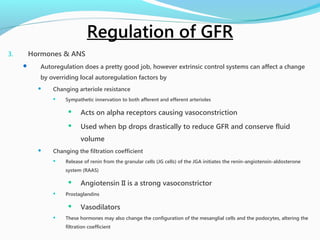
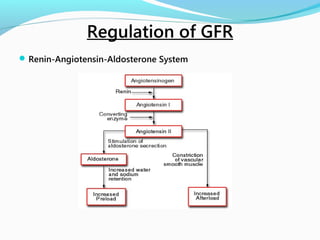
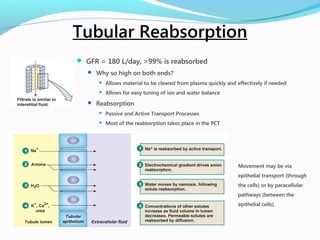
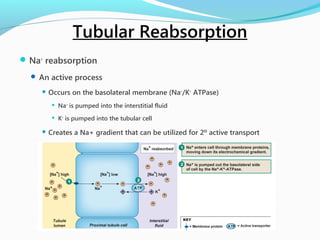
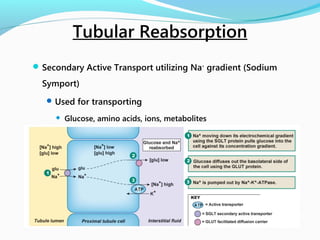
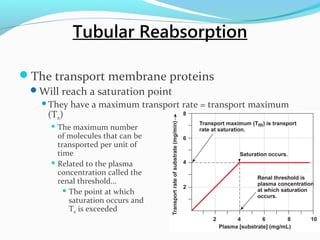
This document provides an overview of renal physiology, including the mechanisms of urine formation through glomerular filtration, tubular reabsorption and secretion. It discusses the locations and processes of filtration, reabsorption and secretion. Specifically, it describes how glomerular filtration occurs due to hydrostatic and oncotic pressures, and how the glomerular filtration rate of 125 mL/min results in 180 L of filtrate per day. It also summarizes the regulation of GFR through myogenic, tubuloglomerular and hormonal mechanisms like the renin-angiotensin-aldosterone system. Finally, it outlines the processes of tubular reabsorption of substances like sodium, glucose and water, as well