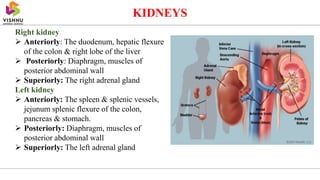
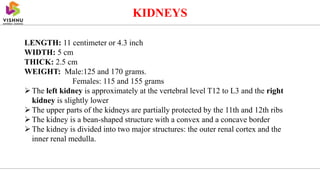
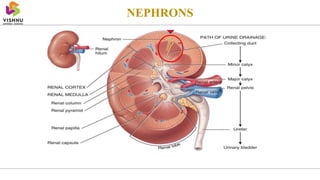
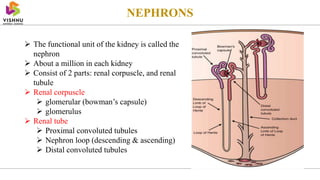
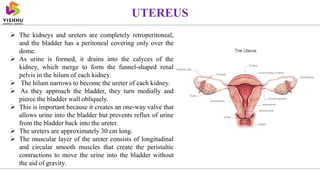
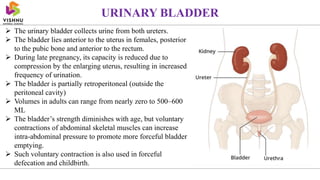
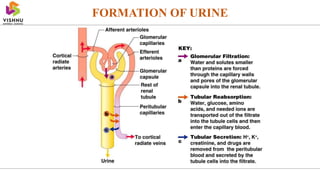
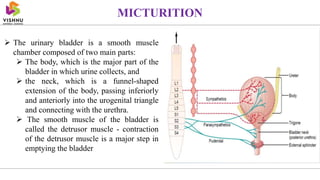
The urinary system consists of the kidneys, ureters, bladder, and urethra. The kidneys filter the blood to remove waste and regulate electrolyte and fluid levels. The nephrons are the functional units of the kidneys that filter blood to form urine. Urine travels from the kidneys through the ureters to the bladder, where it is stored until excreted through the urethra. The urinary system regulates blood volume and pressure and removes waste from the body.