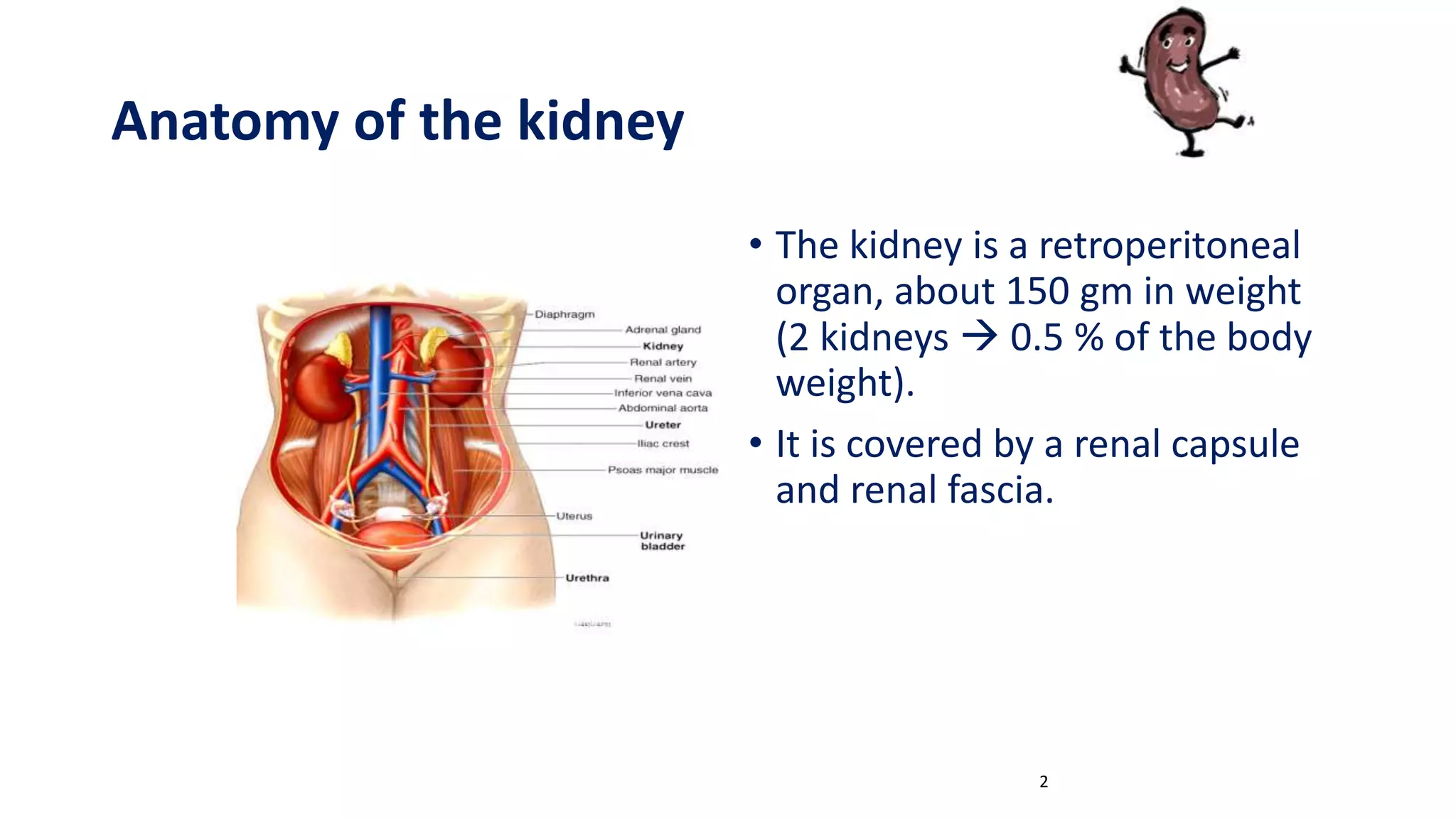
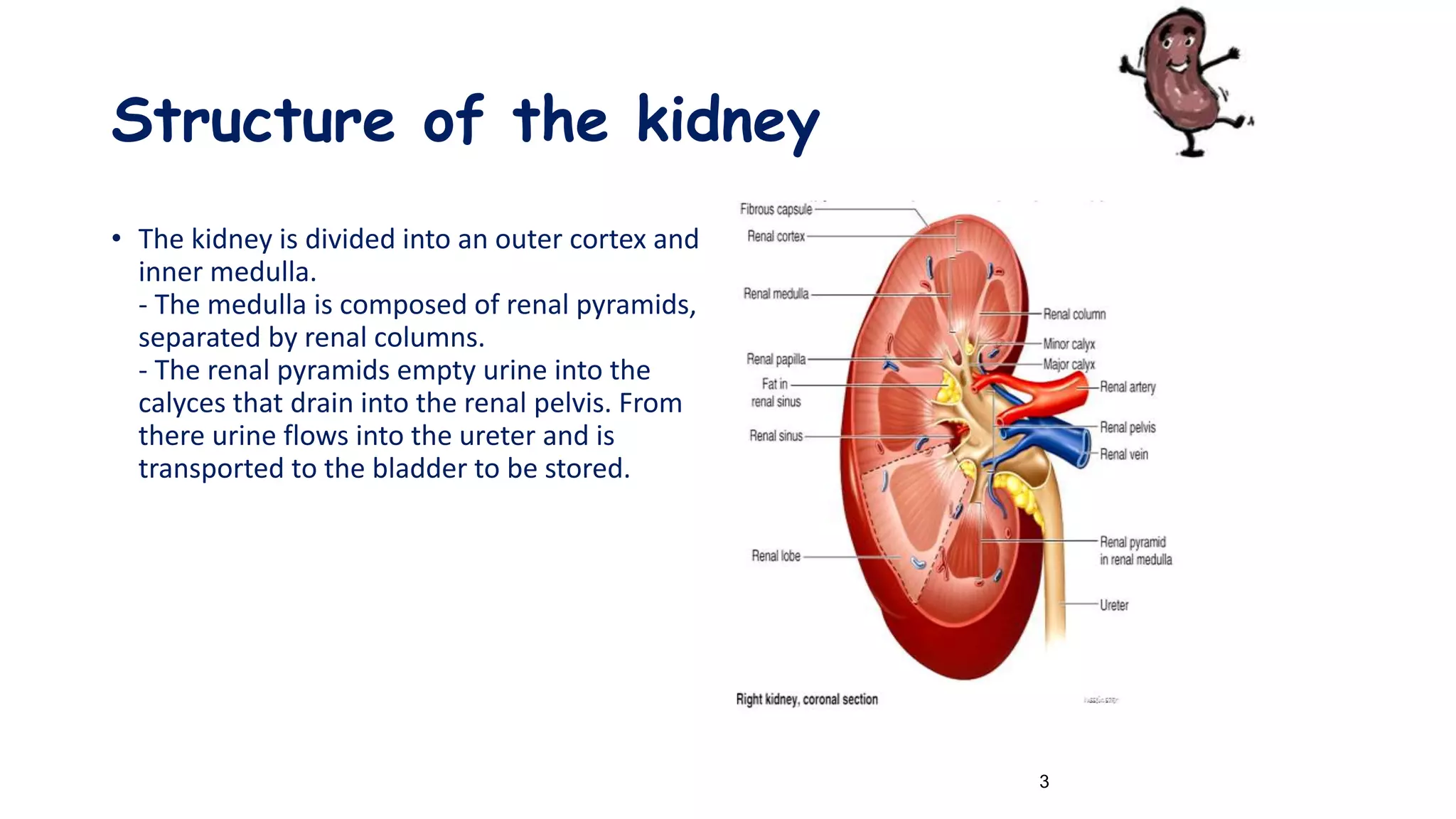
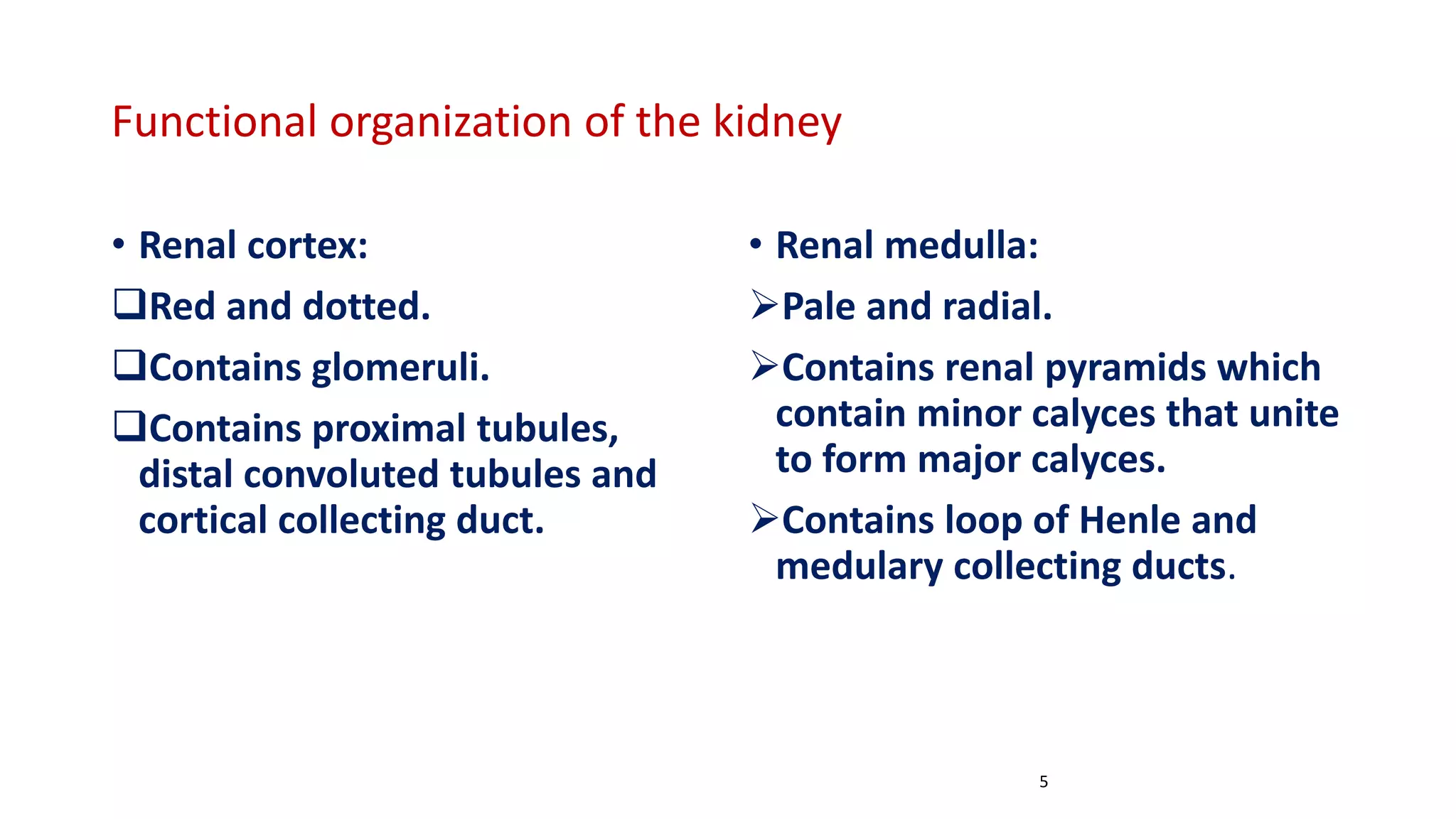
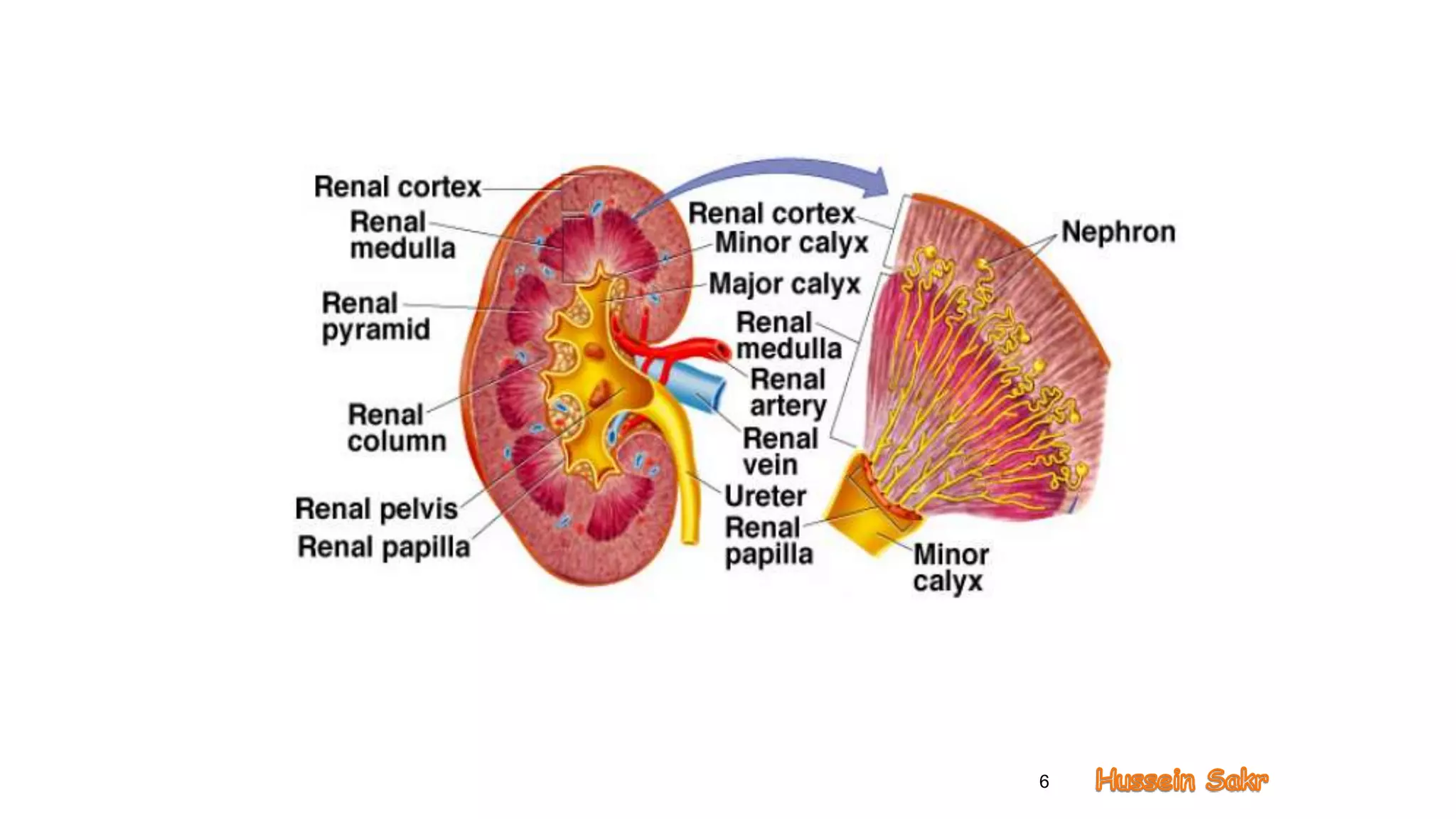
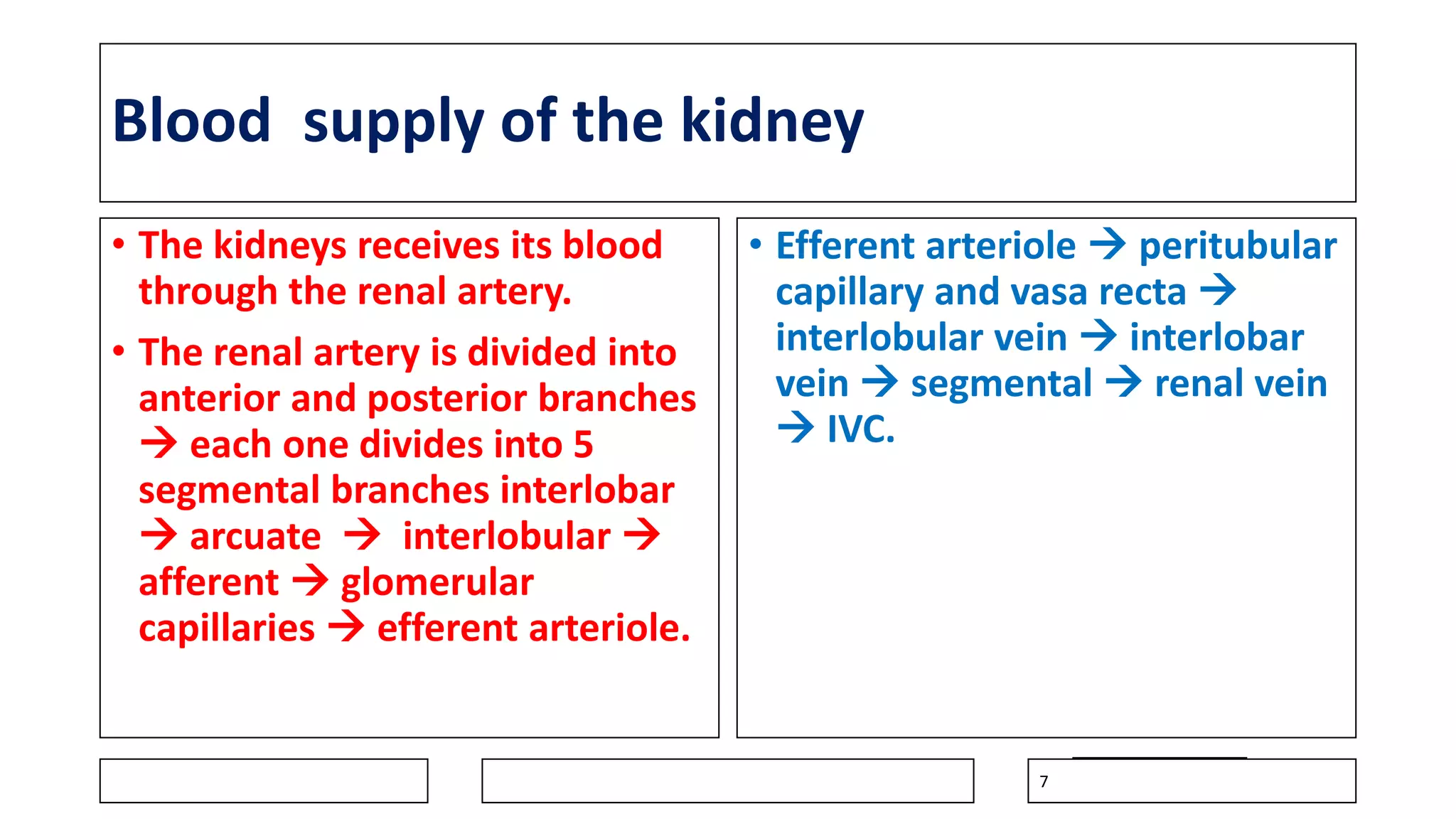
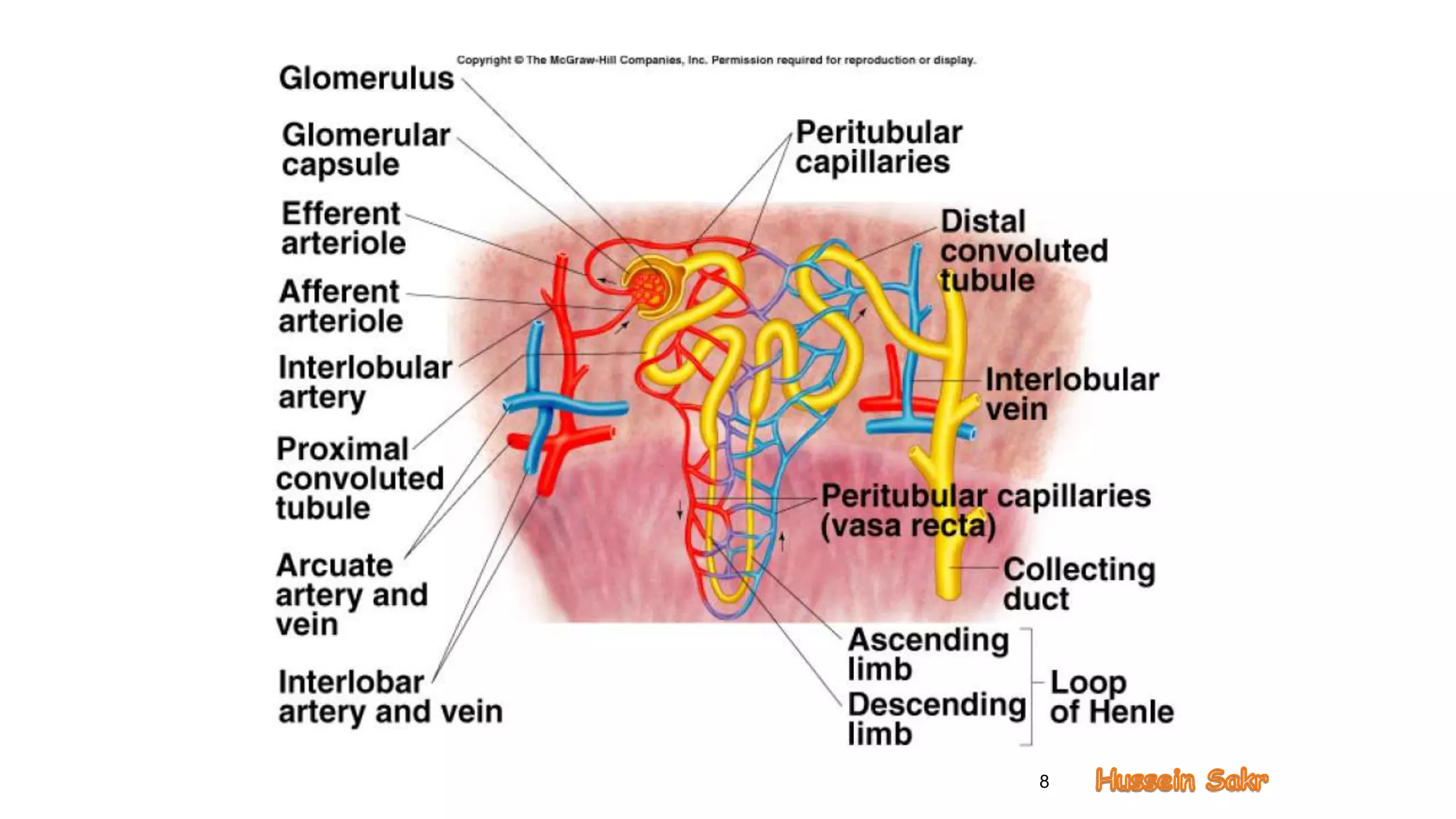
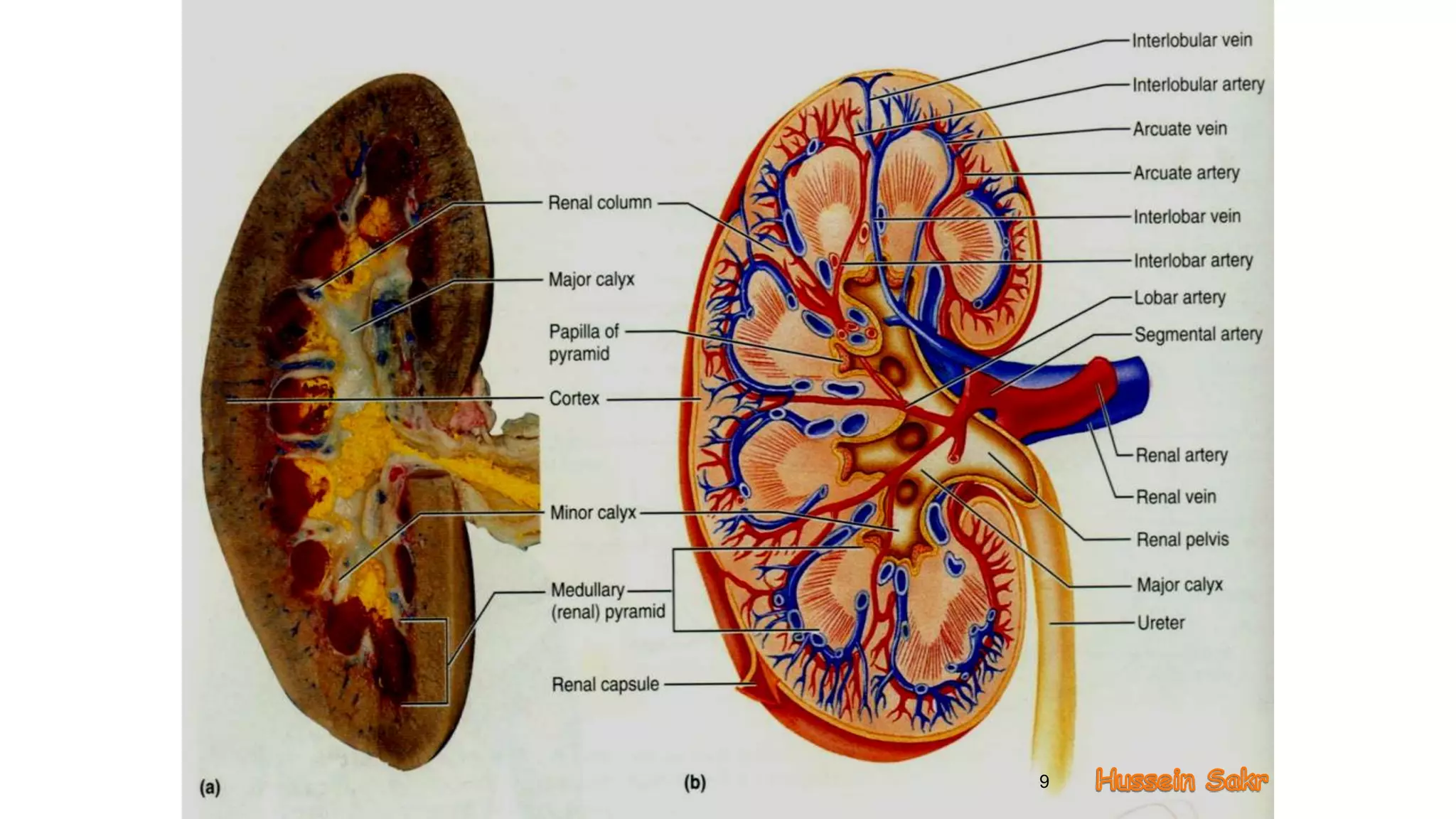
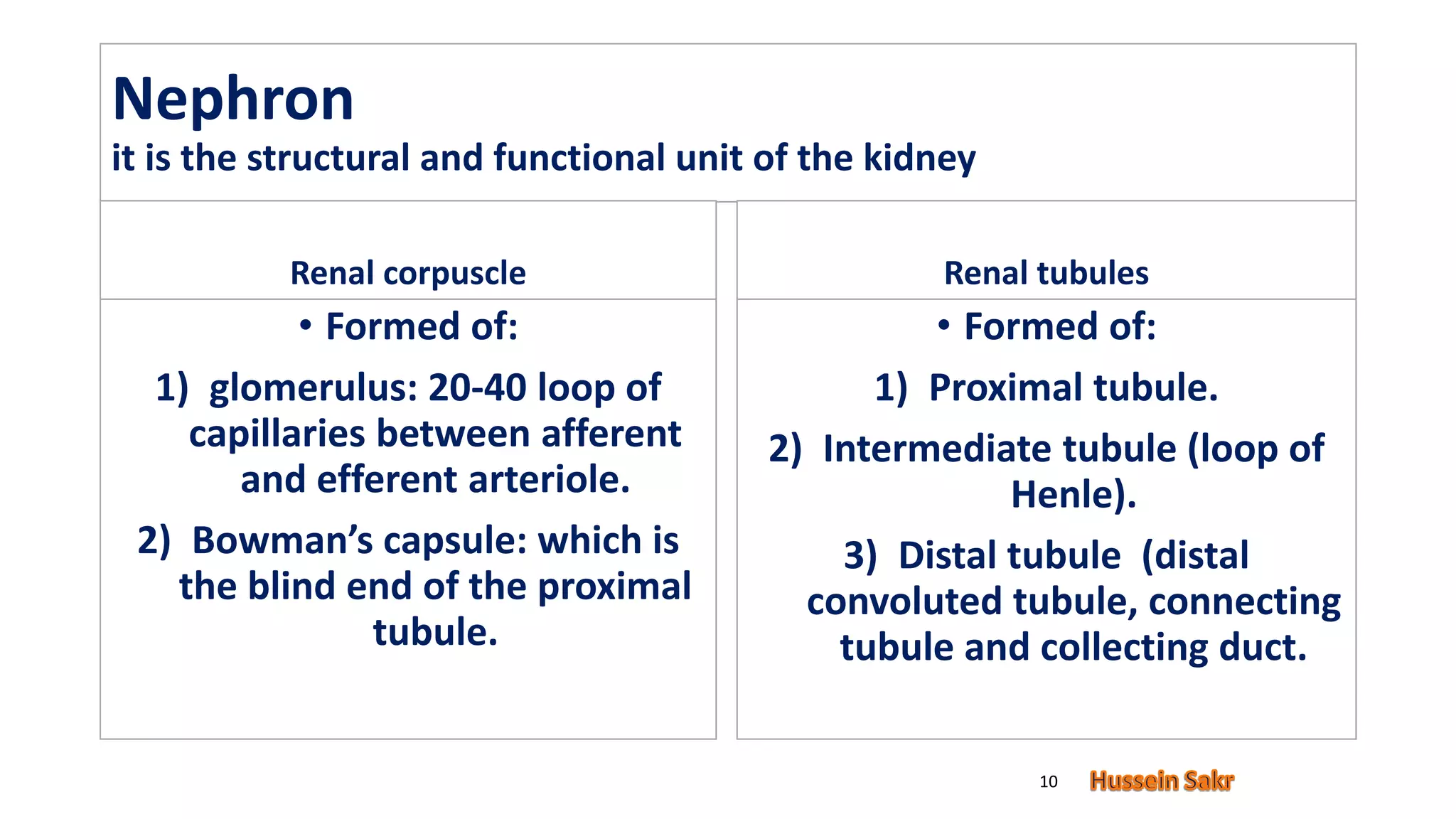
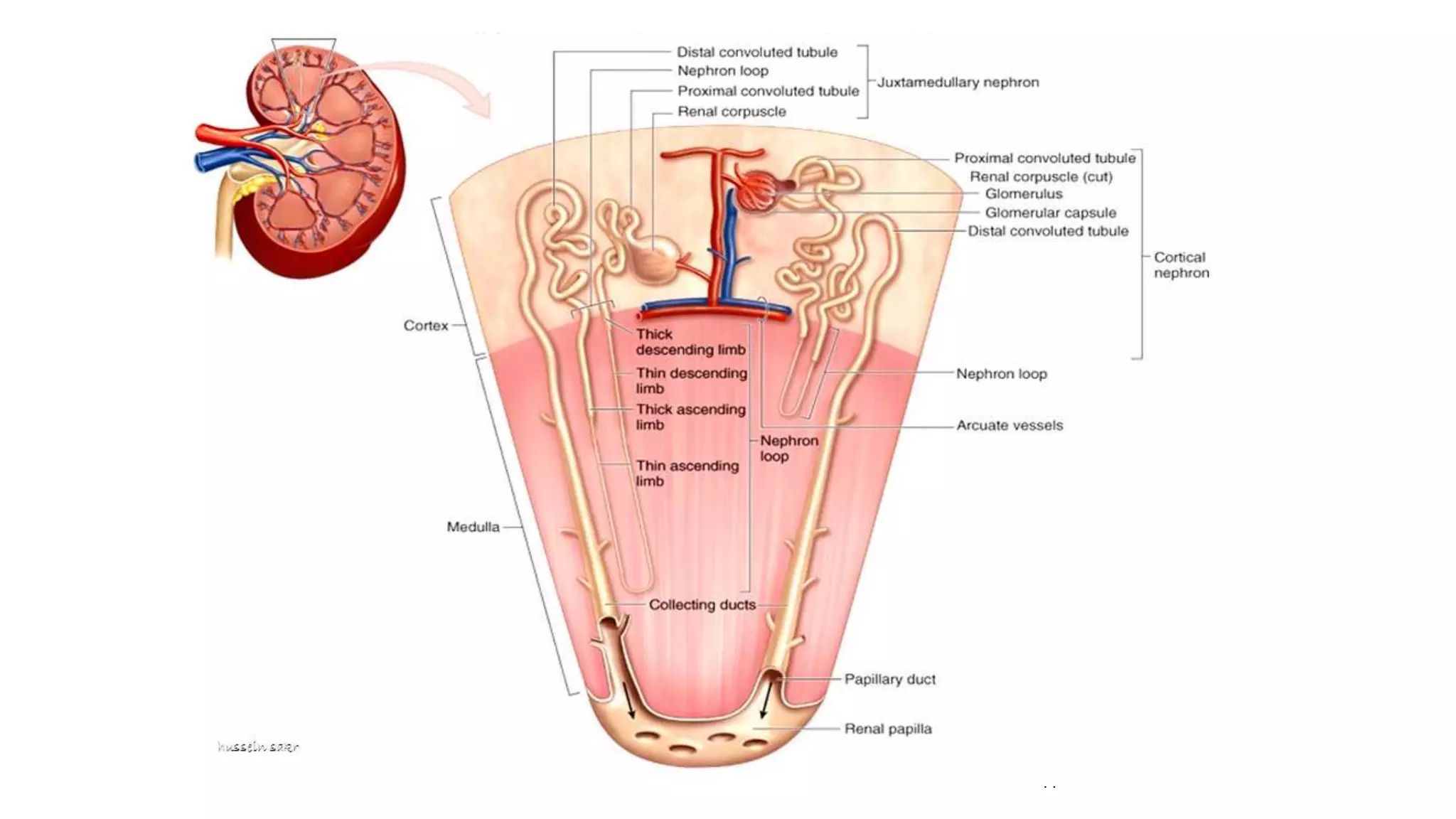
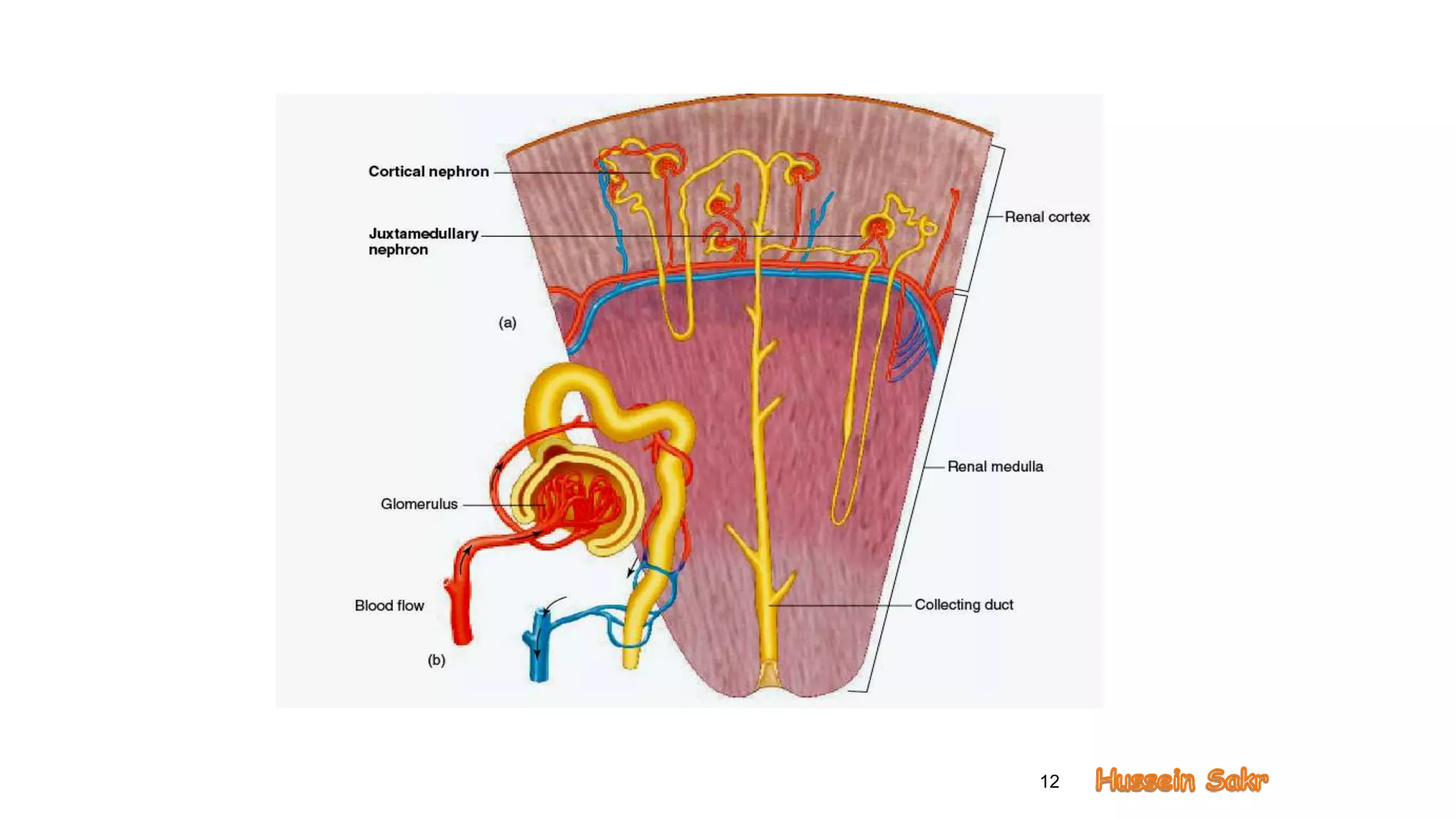
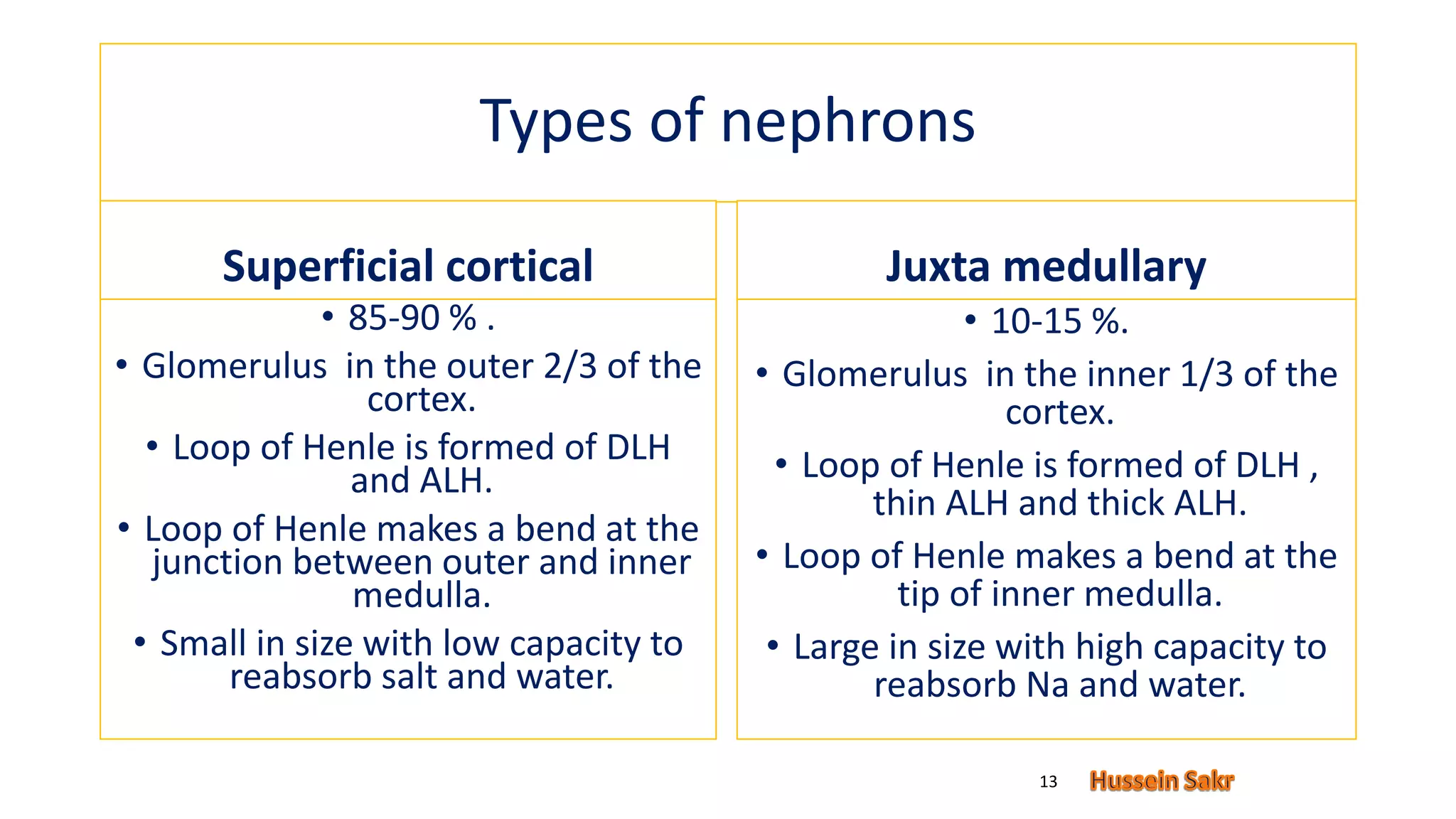
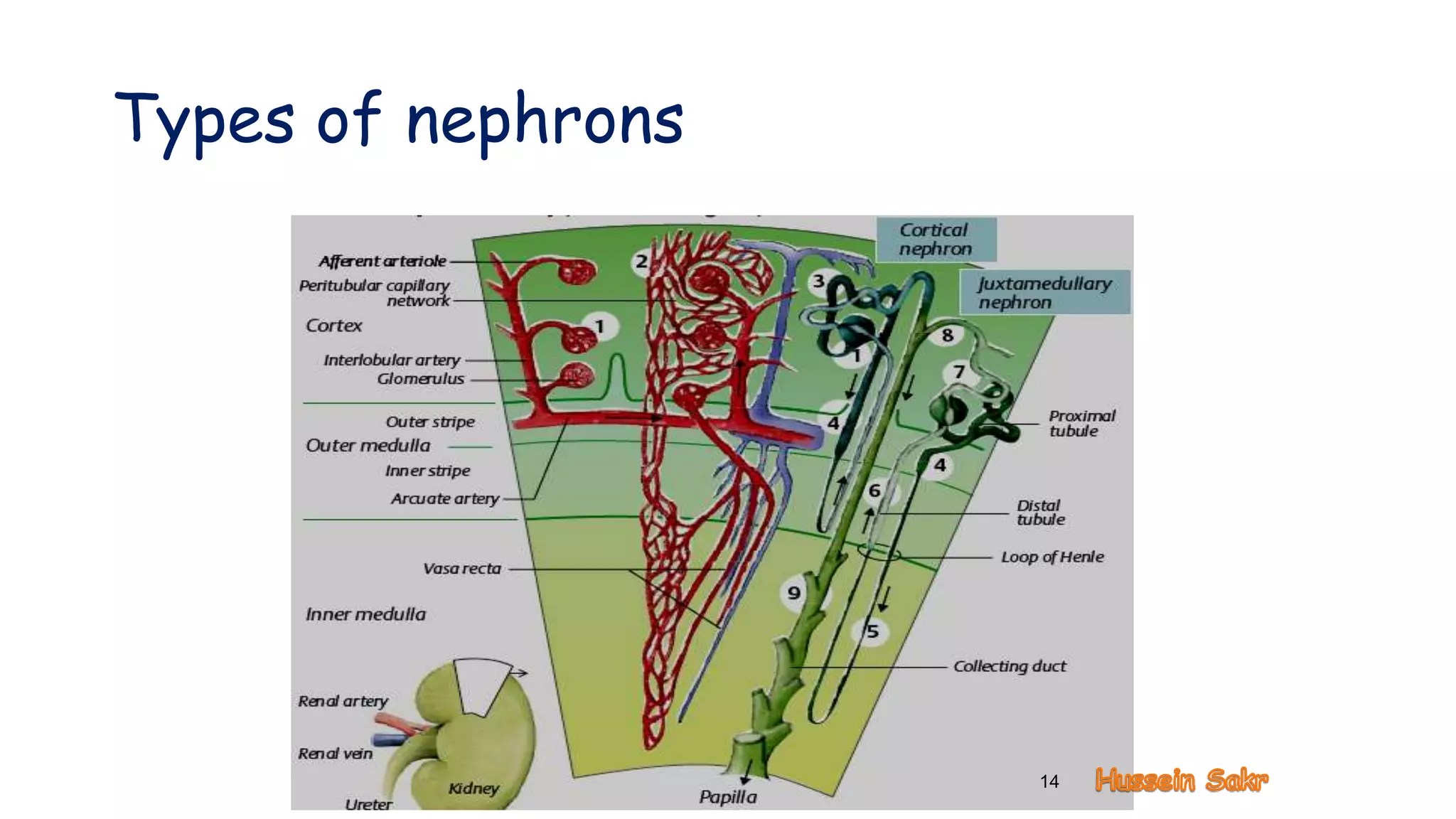
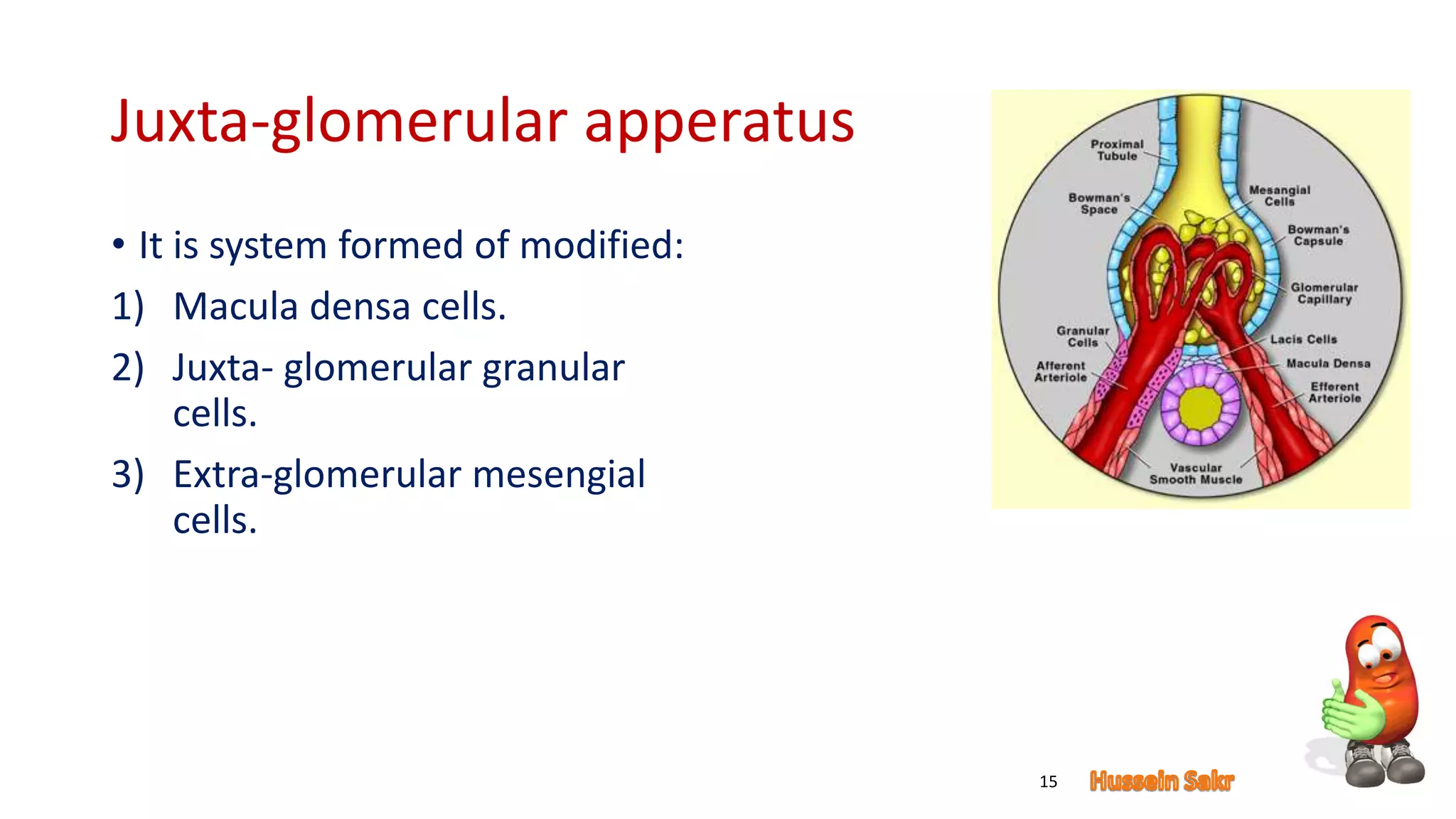
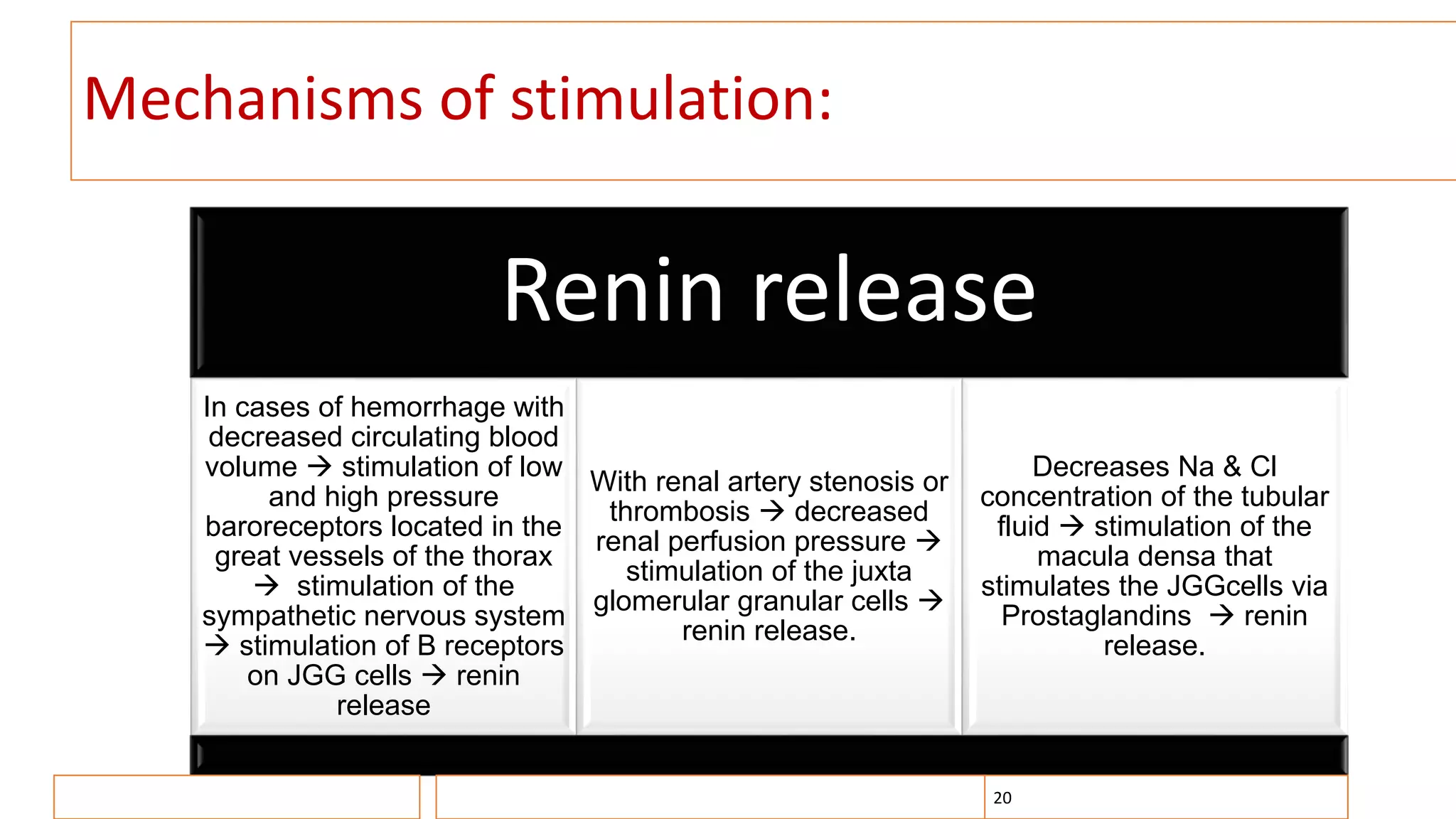
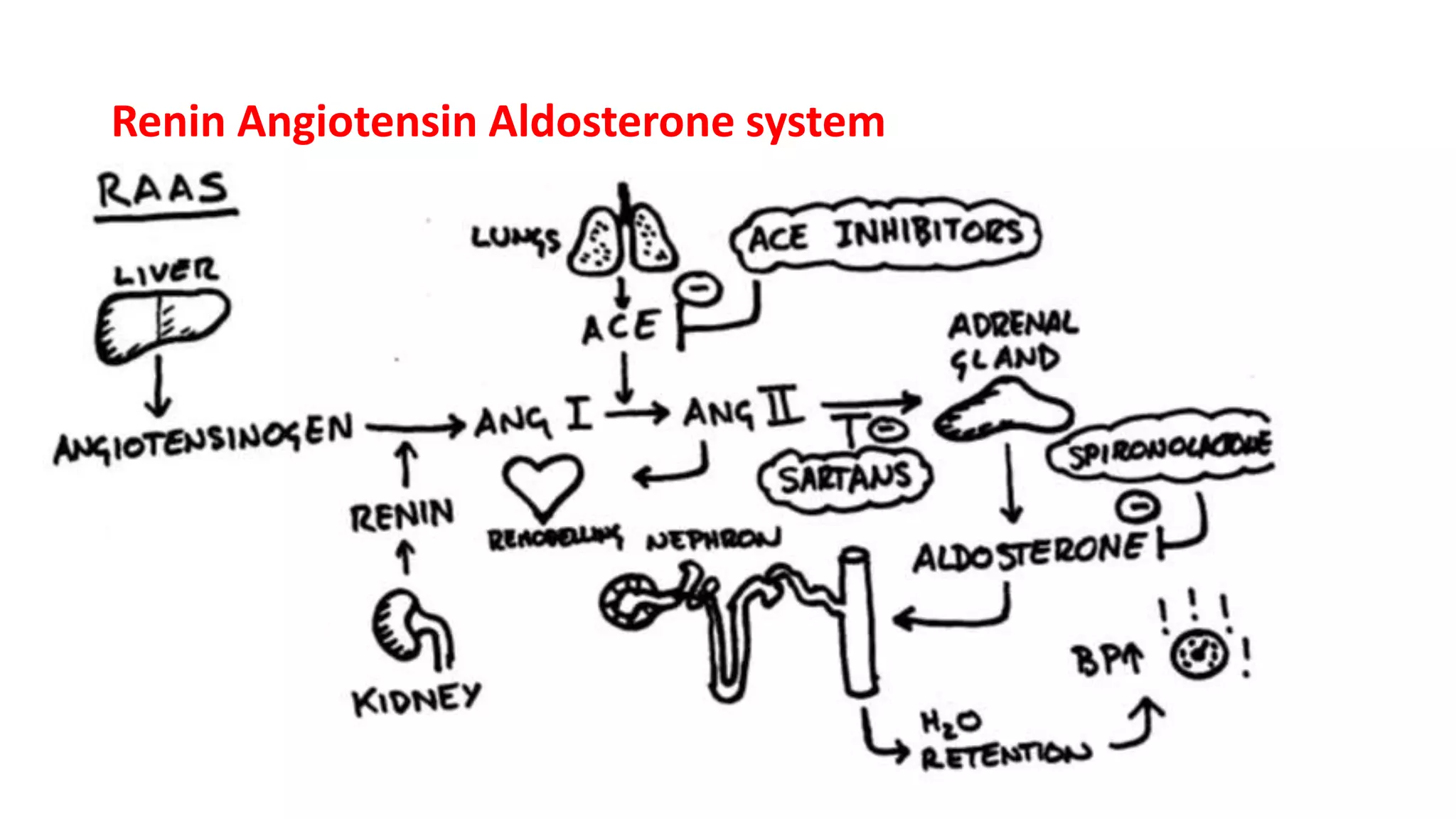
The document provides an overview of renal physiology, including the anatomy, structure, function, and blood supply of the kidney. It describes the nephron as the functional unit of the kidney, composed of the renal corpuscle and renal tubules. There are two main types of nephrons - superficial cortical nephrons and juxtamedullary nephrons. The document also discusses the juxtaglomerular apparatus, which regulates renin release in response to changes in sodium concentration or blood pressure. Renin triggers the renin-angiotensin-aldosterone system, which functions to retain salt and water and constrict blood vessels.