This document provides an overview of renal physiology, covering the following key points in 3 sentences:
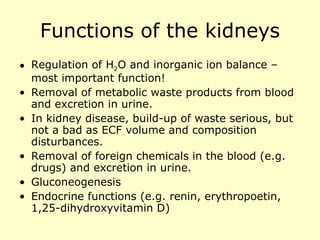
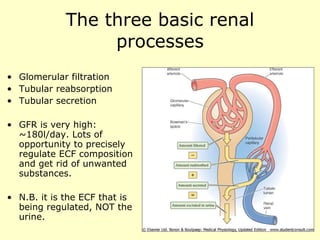
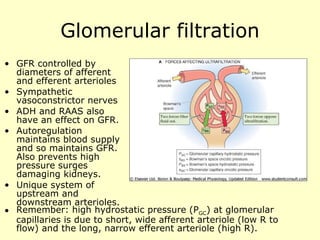
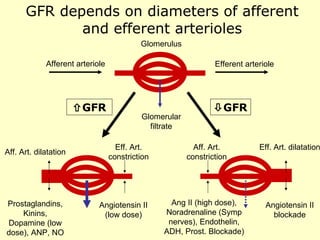
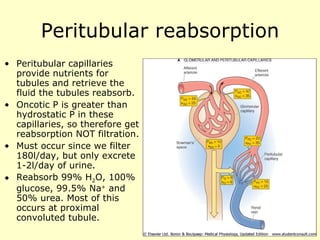
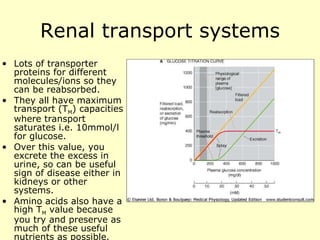
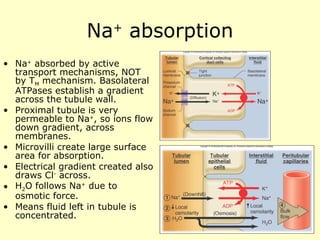
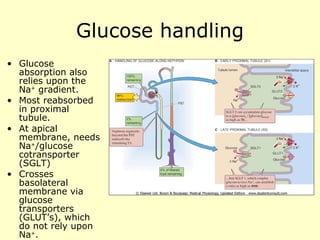
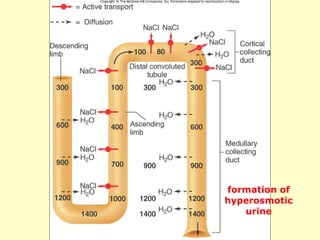
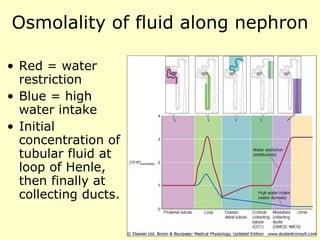
The kidneys have excellent blood supply and filter plasma to remove waste and regulate water/ion balance through processes of glomerular filtration, tubular reabsorption and secretion; the nephron is the functional unit where filtration occurs at the glomerulus and capillaries aid reabsorption; precise control of filtration, reabsorption of substances like sodium, glucose and water, and secretion of potassium allows the kidneys to maintain electrolyte and fluid homeostasis.
![Glomerulus and Bowman’s capsule Glomerular filtrate drains into Bowman’s space, and then into proximal convoluted tubule. Endothelium has pores to allow small molecules through. Podocytes have negative charge. This and the basement membrane stops proteins getting through into tubular fluid. Macula densa senses GFR by [Na + ] Juxtaglomerular (JG) apparatus includes JG cells that secrete renin. JGA helps regulate renal blood flow, GFR and also indirectly, modulates Na + balance and systemic BP](https://image.slidesharecdn.com/renalphysiologyintroduction-100717035925-phpapp02/85/Renal-physiology-introduction-5-320.jpg)
![Modulation of K + secretion Luminal factors Stimulators Inhibitors Flow rate [K + ] [Na + ] [Cl - ] [Cl - ] [Ca 2+ ] [HCO 3 - ] Ba 2+ -ve luminal voltage Amiloride Selected Diuretics Peritubular Factors Stimulators Inhibitors K + intake pH [K + ] Adrenaline pH Aldosterone ADH](https://image.slidesharecdn.com/renalphysiologyintroduction-100717035925-phpapp02/85/Renal-physiology-introduction-17-320.jpg)
![Urea recycling Urea toxic at high levels, but can be useful in small amounts. Urea recycling causes buildup of high [urea] in inner medulla. This helps create the osmotic gradient at loop of Henle so H 2 O can be reabsorbed.](https://image.slidesharecdn.com/renalphysiologyintroduction-100717035925-phpapp02/85/Renal-physiology-introduction-22-320.jpg)