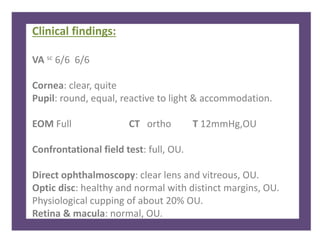
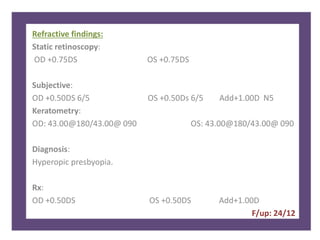
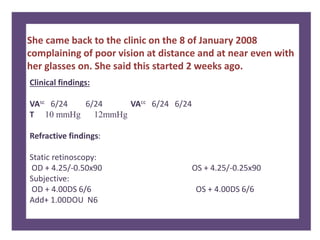
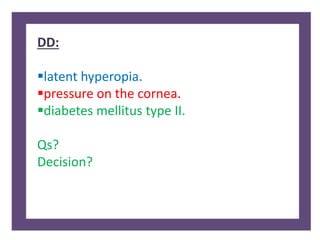
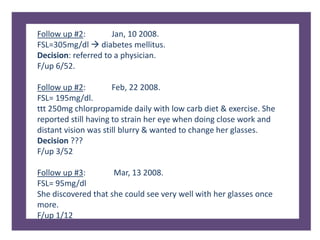
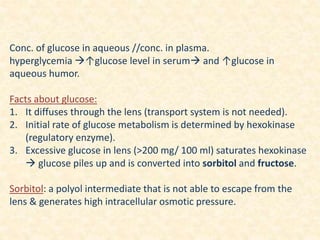
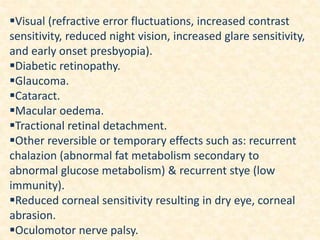
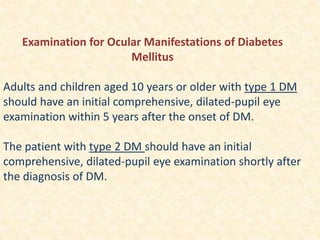
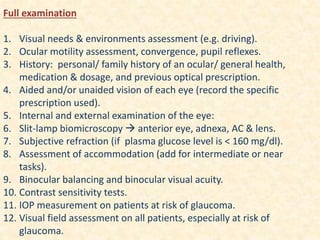
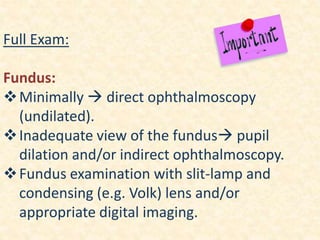
A 41-year-old female presented with difficulty reading small prints and using her cellphone for 6 months. She was diagnosed with hyperopic presbyopia but returned with worsening vision. Her blood sugar was found to be elevated, diagnosing her with diabetes mellitus. Diabetes can cause refractive changes, cataracts, and retinopathy due to physiological changes in the eye. A full ocular examination is important for managing diabetic patients.