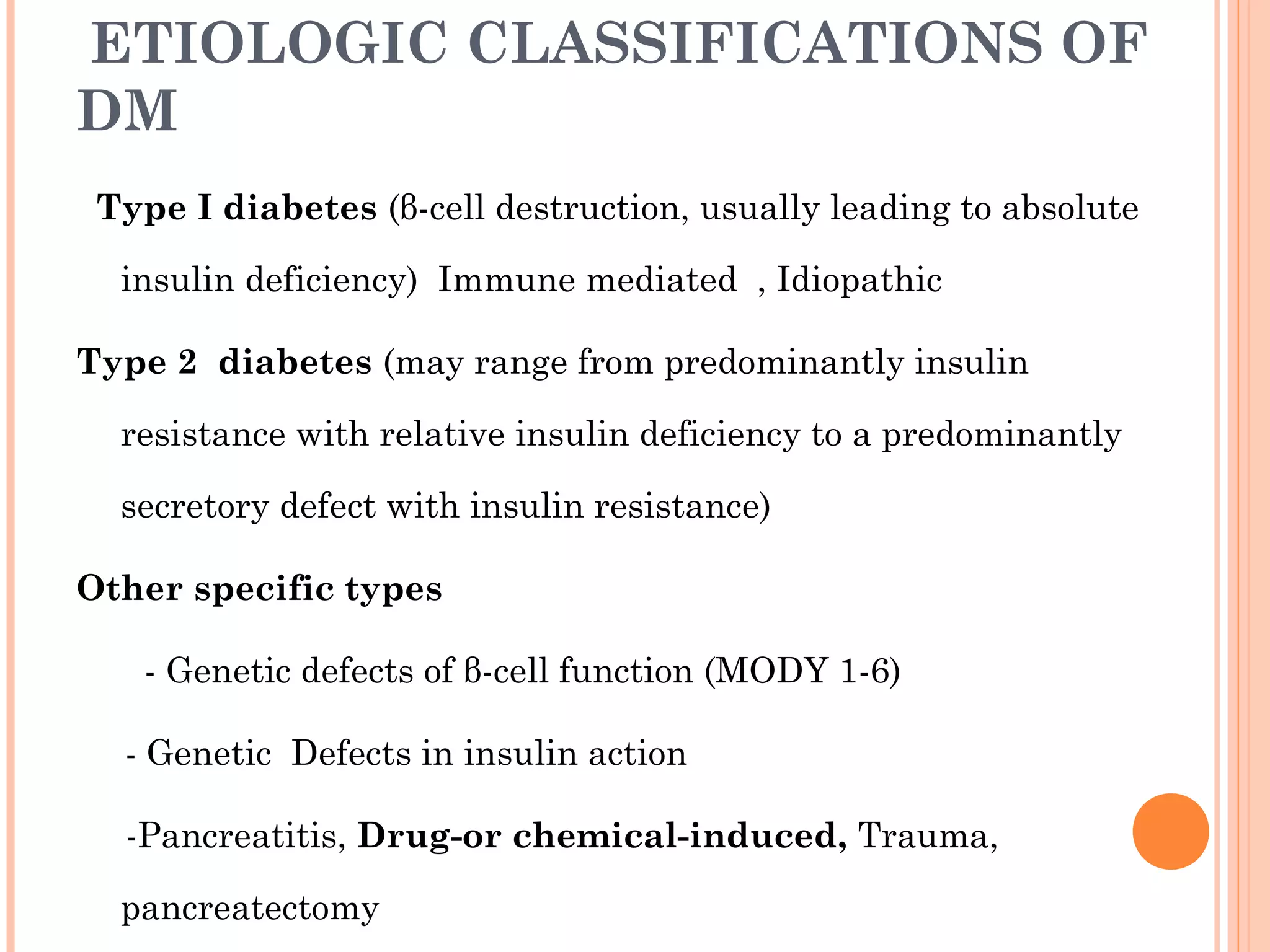
1. Diabetes mellitus is a chronic metabolic disease characterized by hyperglycemia due to either lack of insulin production or insulin resistance. The two main types are type 1 DM caused by autoimmune destruction of insulin-producing beta cells, and type 2 DM caused by insulin resistance with relative insulin deficiency.
2. Symptoms of diabetes include increased thirst, frequent urination, and unexplained weight loss. Type 1 diabetes often presents with diabetic ketoacidosis, while type 2 diabetes is usually diagnosed through routine testing. Treatment involves lifestyle changes, oral medications, and sometimes insulin therapy to control blood glucose levels.
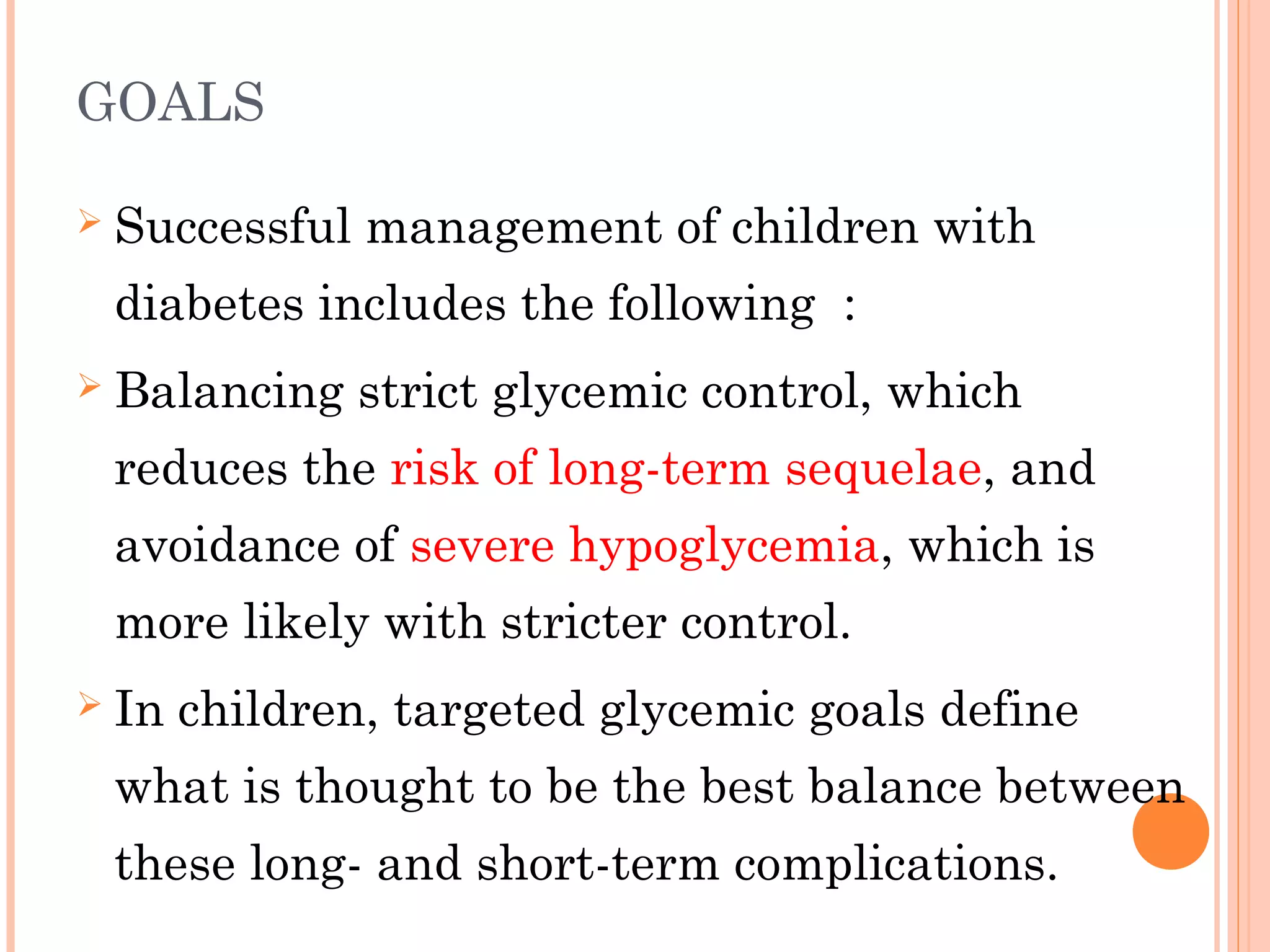
3. Strict control is important to prevent long-term complications affecting the eyes, kidneys, nerves, heart