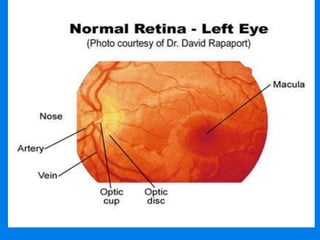
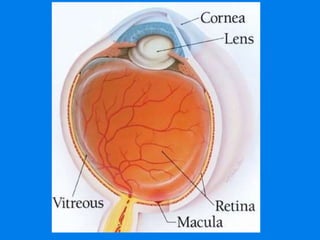
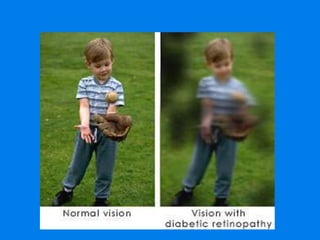
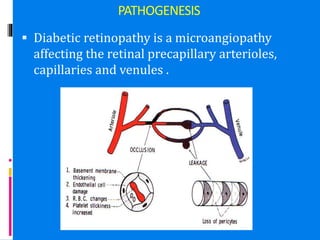
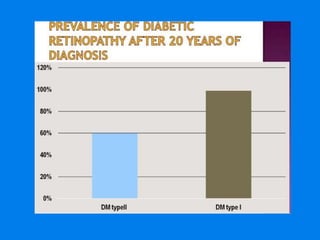
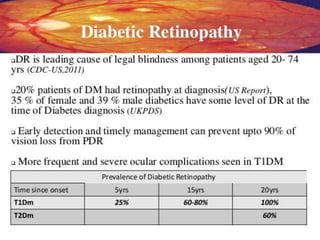
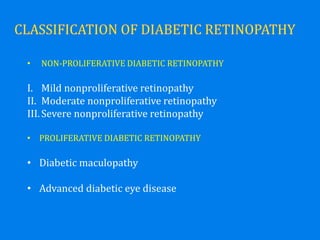
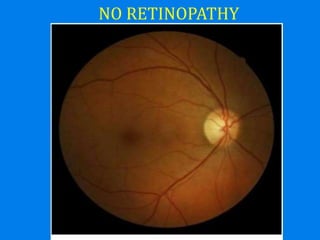
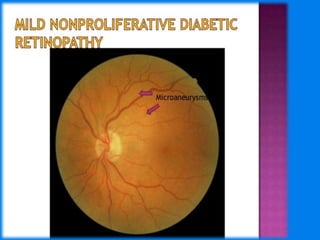
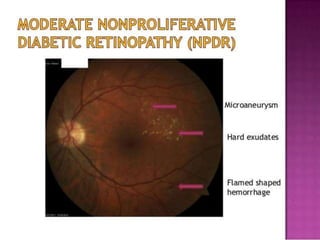
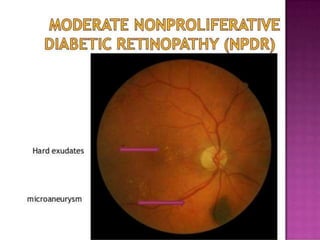
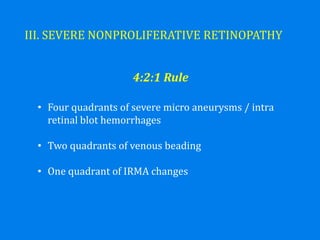
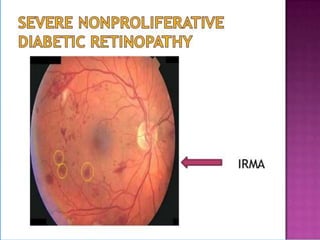
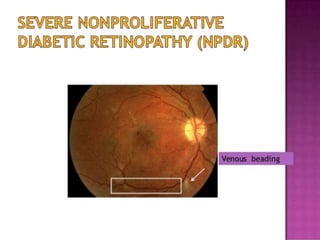
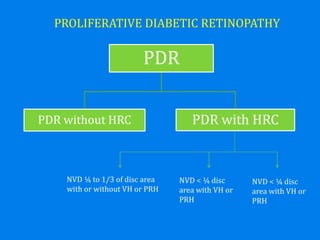
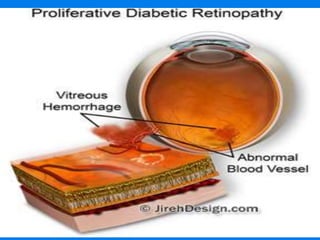
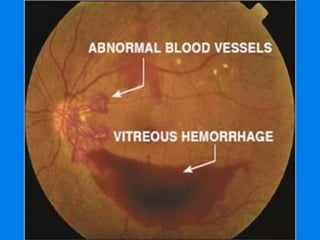
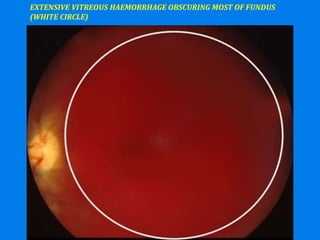
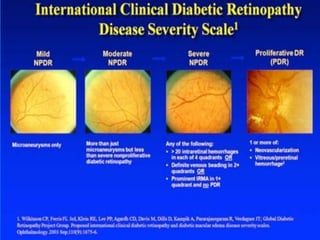
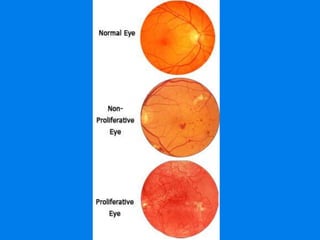
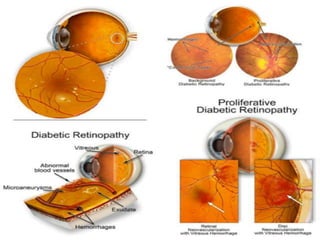
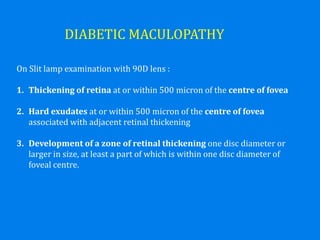
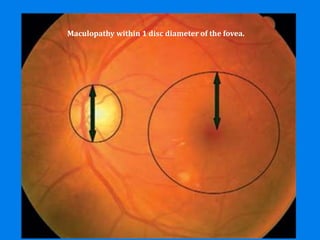
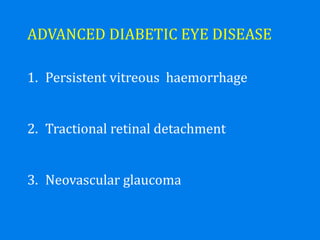
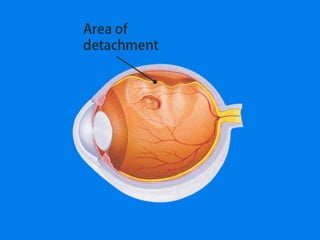
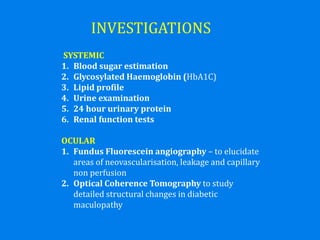
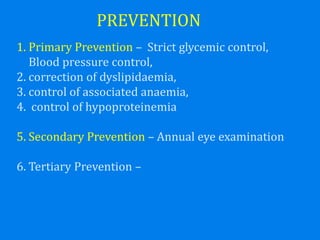
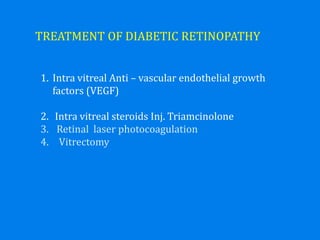
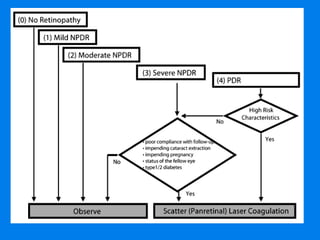
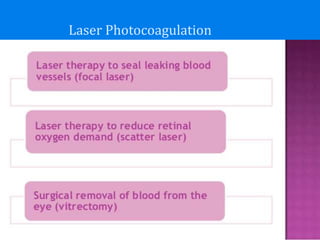
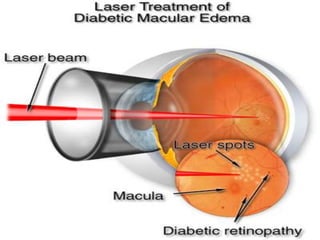
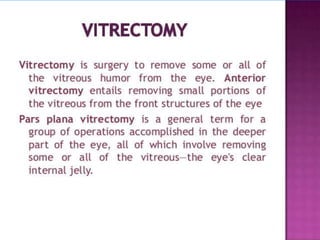
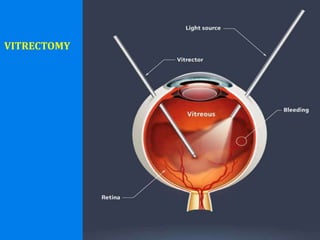
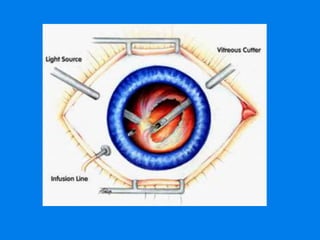
This document discusses diabetic retinopathy, describing the different types and stages of the disease from mild non-proliferative to proliferative retinopathy. It outlines the pathogenesis as a microangiopathy affecting the retinal blood vessels caused by chronic hyperglycemia. Risk factors and diagnostic investigations like fundus fluorescein angiography and OCT are mentioned. Treatment options discussed include intravitreal anti-VEGF injections, laser photocoagulation, and vitrectomy. Strict glycemic and blood pressure control can help prevent and slow the progression of this complication of diabetes.