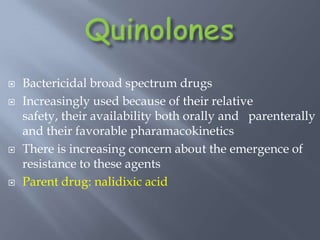
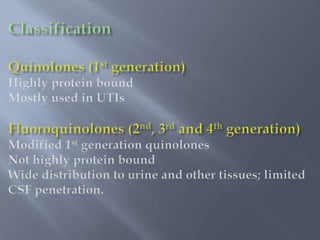
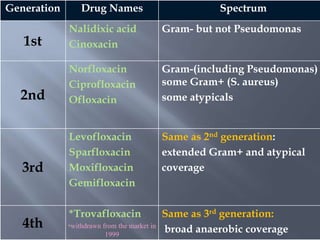
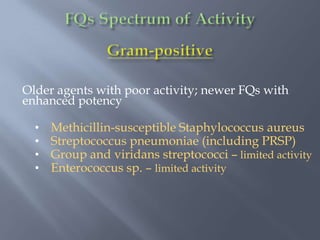
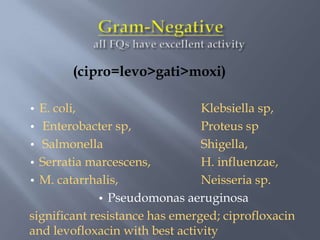
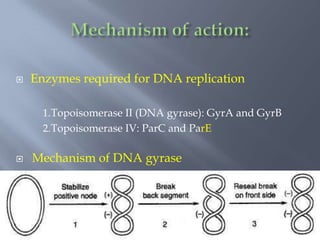
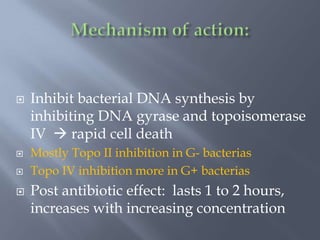
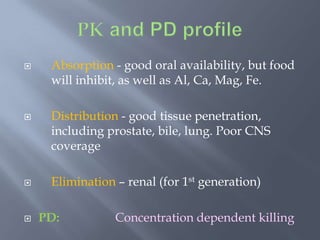
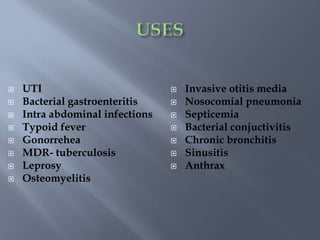
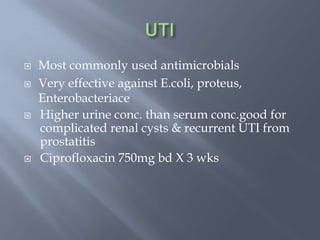
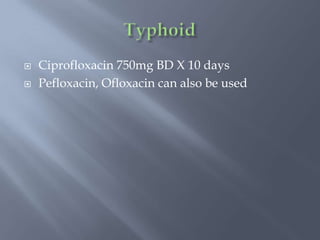
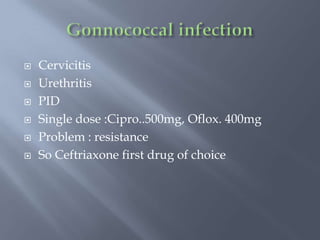
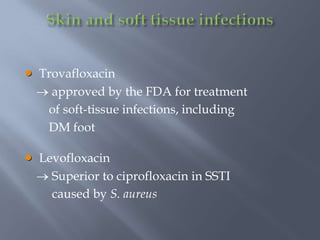
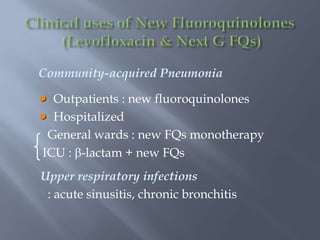
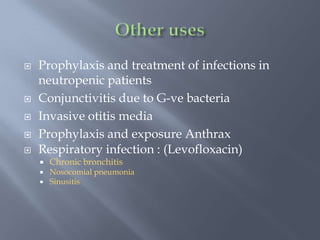
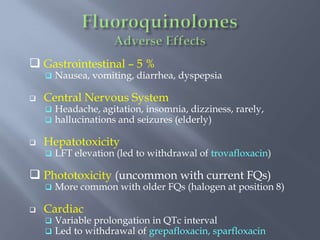
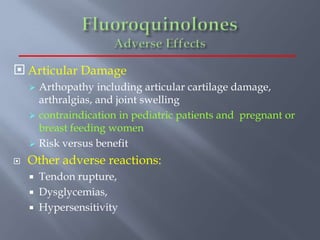
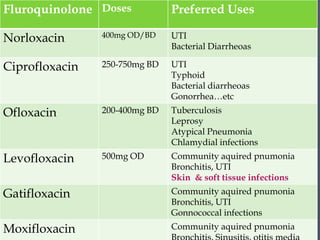
This document discusses fluoroquinolone antibiotics. It describes their spectrum of activity, mechanism of action, pharmacokinetics, uses, and adverse effects. Fluoroquinolones are broad-spectrum antibacterial drugs used commonly due to their oral availability and favorable pharmacokinetics. However, there is increasing concern about emerging resistance. Common fluoroquinolones discussed include norfloxacin, ciprofloxacin, ofloxacin, levofloxacin, and moxifloxacin.