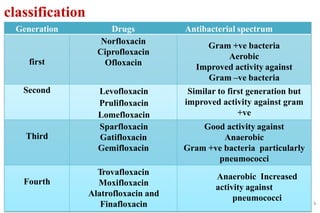
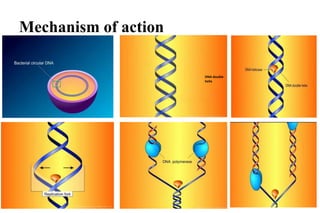
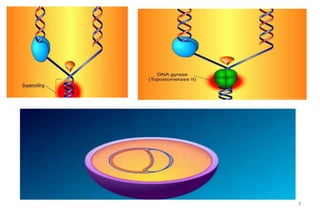
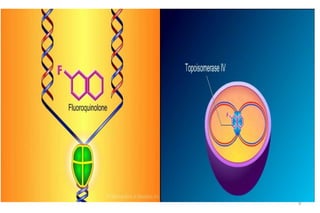
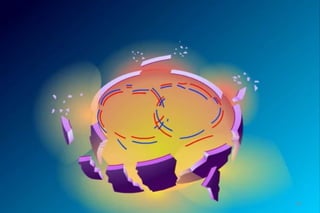
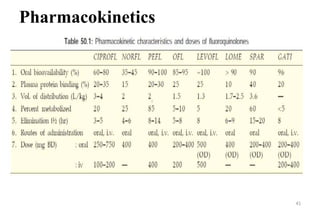
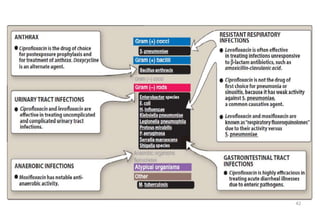
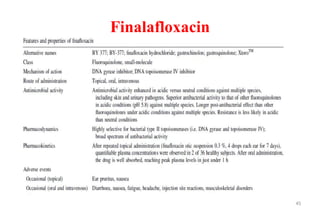
This document provides an overview of quinolones, a class of antibacterial agents. It discusses the discovery of nalidixic acid, the first quinolone, and the subsequent development of fluoroquinolones. The mechanisms of action and mechanisms of resistance are described. Various generations of fluoroquinolones are classified and their spectra of activity, pharmacokinetics, uses, and adverse effects are summarized. Newer quinolone agents such as finalafloxacin and delafloxacin are also briefly mentioned.



![Delafloxacin(June 2017 )
• Delafloxacin was developed by Melinta Therapeutics
• Delafloxacin is used to treat acute bacterial skin and skin
structure infections caused by designated susceptible bacteria.
• Susceptible bacteria are:
• Gram-positive organisms: Staphylococcus aureus (including
methicillin-resistant [MRSA] and methicillin-susceptible
[MSSA] isolates), Staphylococcus haemolyticus, Staphylococcus
lugdunensis, Streptococcus agalactiae, Streptococcus
anginosus group, Streptococcus pyogenes, and Enterococcus
faecalis
• Gram-negative organisms: Escherichia coli, Enterobacter
cloacae, Klebsiella pneumoniae, and Pseudomonas aeruginosa.
46](https://image.slidesharecdn.com/quinolones-200315164905/85/Quinolones-and-fluroquinolones-46-320.jpg)