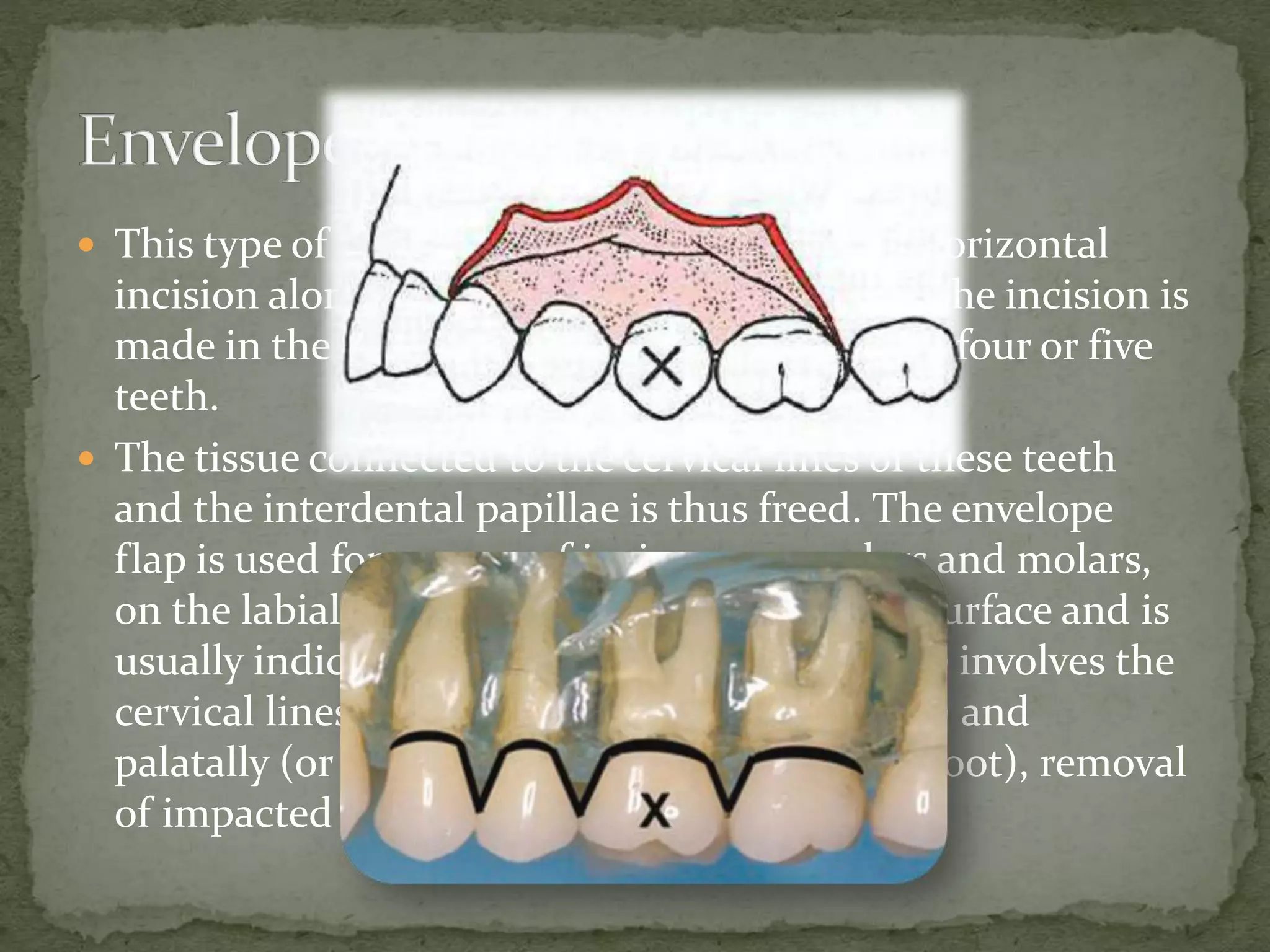
This document discusses various aspects of oral surgery preparation and procedures. It covers definitions of oral surgery, pre-surgical evaluation and preparation, asepsis and sterilization techniques, surgical staff preparation, incision types, flap design principles, tissue handling techniques, hemostasis, suturing, wound decontamination and debridement, and edema control. The document provides details on each topic to thoroughly outline the process of oral surgery.