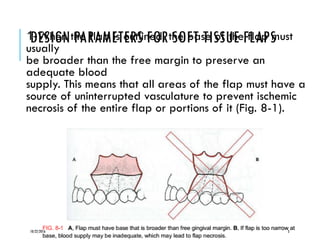
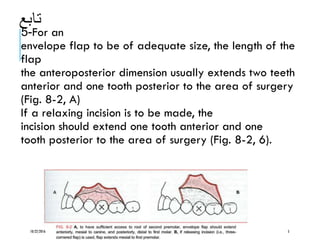
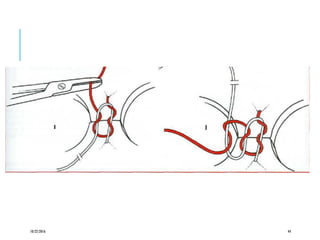
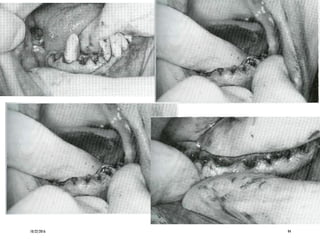
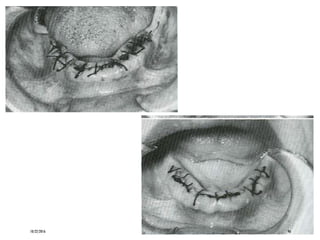
This document discusses principles of soft tissue flap design, development, and management for oral surgical procedures. It covers key aspects of flap design such as ensuring adequate blood supply to the flap, sufficient size for access and retraction, and full thickness reflection. Specific flap incisions are described like envelope, three-cornered, and four-cornered flaps. Techniques for developing flaps like incising and reflecting with elevators are covered. Principles of suturing flaps are also summarized such as coapting wound margins, hemostasis, and knot tying. Common suture materials, sizes and techniques are outlined.
![PRINCIPLES OF FLAP DESIGN, DEVELOPMENT,
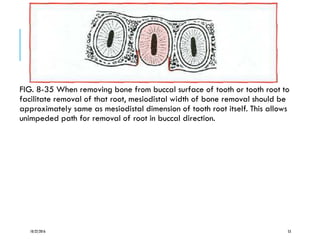
AND MANAGEMENT:
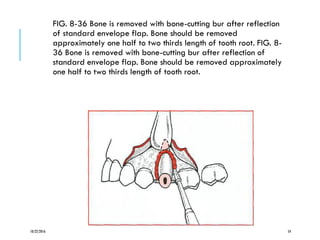
The term local flap indicates a section of soft tissue that
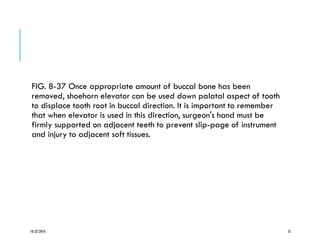
(1) is outlined by a surgical incision, (2) carries its own]
blood supply, (3) allows surgical access to underlying
tissues, (4) can be replaced in the original position, and (5]
can be maintained with sutures and is expected to heal,
Soft tissue flaps are frequently used in oral surgical,
periodontic, and endodontic procedures to gain access to
underlying tooth and bone structures. To perform a tooth
extraction properly the dentist must have a clear
understanding of the principles of design, development,
and
management of soft tissue flaps.
10/22/2016 2](https://image.slidesharecdn.com/ch8c-161022145512/85/Principles-of-more-complex-exdontia-By-Cezar-Edward-2-320.jpg)