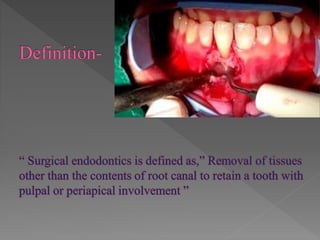
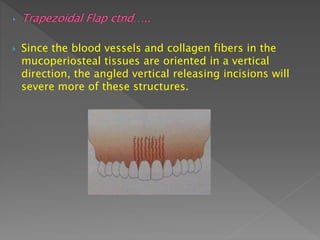
This document provides an overview of endodontic surgery and its concepts. It discusses the history and evolution of endodontic surgery techniques. It also covers indications for endodontic surgery, classifications of different surgical procedures, and considerations for pre-surgical treatment planning. Key surgical steps like flap design, osteotomy, and root-end resection are summarized.












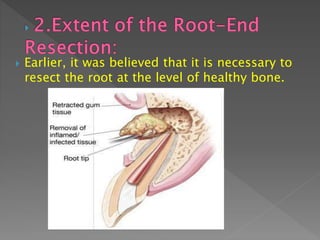

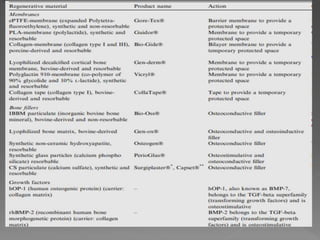



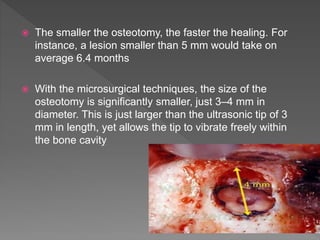
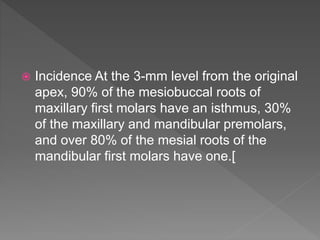
![ Von Arx et al.[13] recommended a resection of the
apical 3 mm, followed by the preparation of a
root-end cavity 3 mm deep, making the “therapeutic
length” 6 mm.
Hess found out that that resecting 1 mm off the
apex reduces 52% of apical ramifications and 40%
of lateral canals; 2 mm off the apex reduces 78% of
apical ramifications and 86% of lateral canals.
Three millimeters off the apex reduces 93% of
apical ramifications and 98% of lateral canals.[](https://image.slidesharecdn.com/surgicalendodontics-140923071441-phpapp02-180328182419/85/endodontic-surgery-and-its-current-concepts-95-320.jpg)



![ Ananad S, Soujanya E, Raju A, Swathi A. Endodontic microsurgery:
An overview. Dent Med Res [serial online] [cited 2018 Mar 27];3:31-
7. Available from:
http://www.dmrjournal.org/text.asp?2015/3/2/31/159172
https://www.aae.org/specialty/wp-
content/uploads/sites/2/2017/07/ecfefall2010final.pdf](https://image.slidesharecdn.com/surgicalendodontics-140923071441-phpapp02-180328182419/85/endodontic-surgery-and-its-current-concepts-115-320.jpg)
