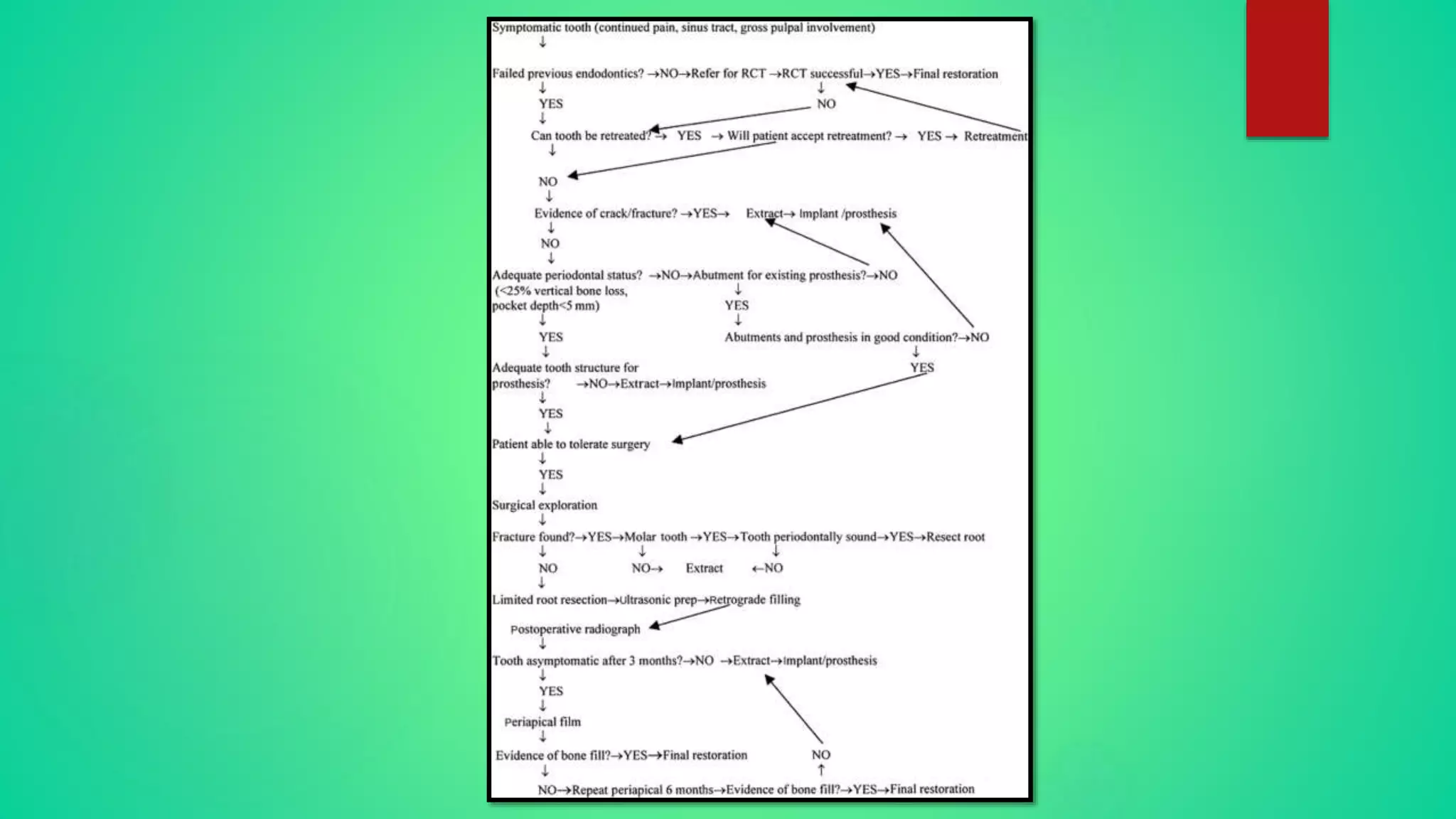
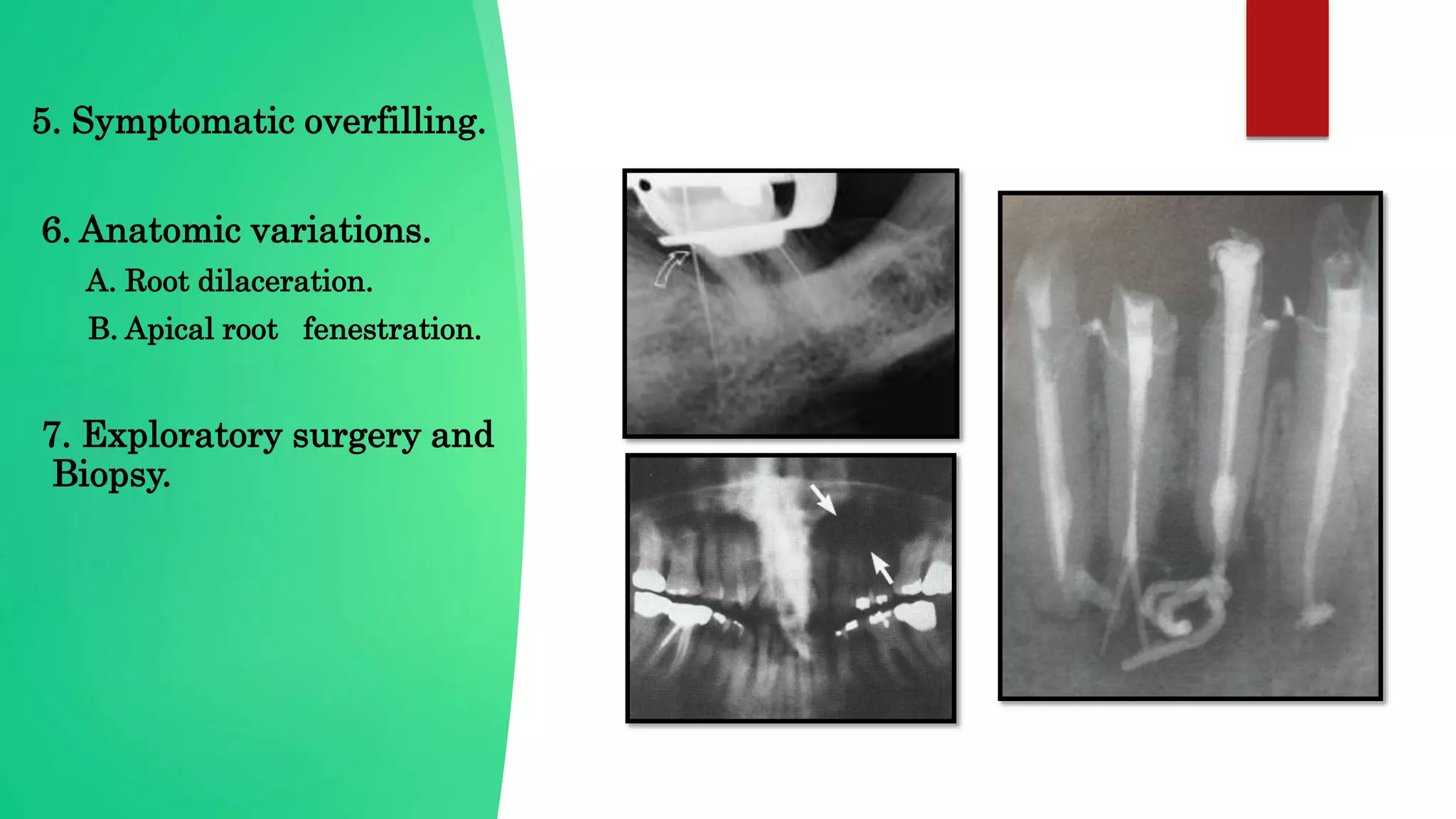
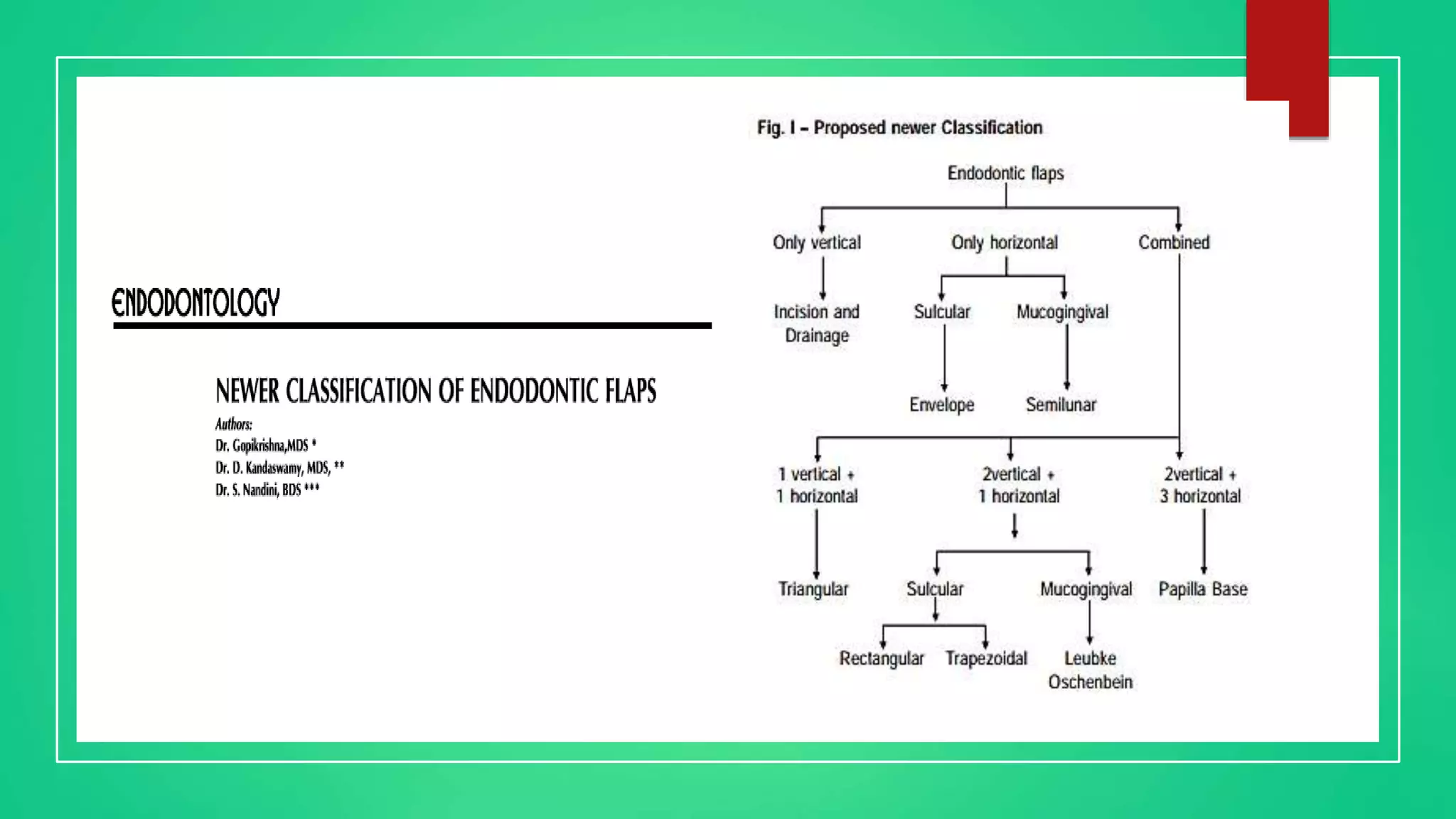
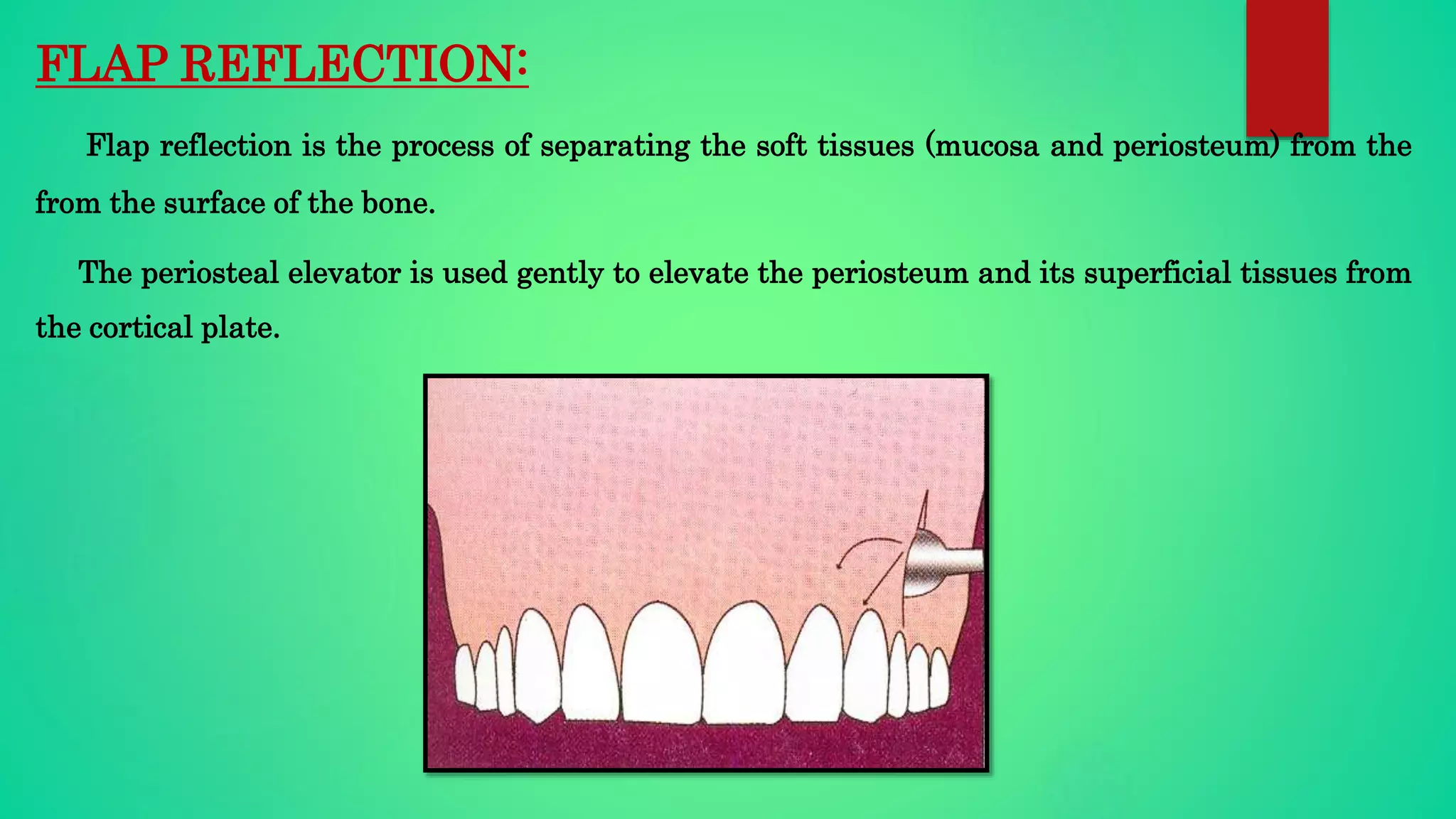
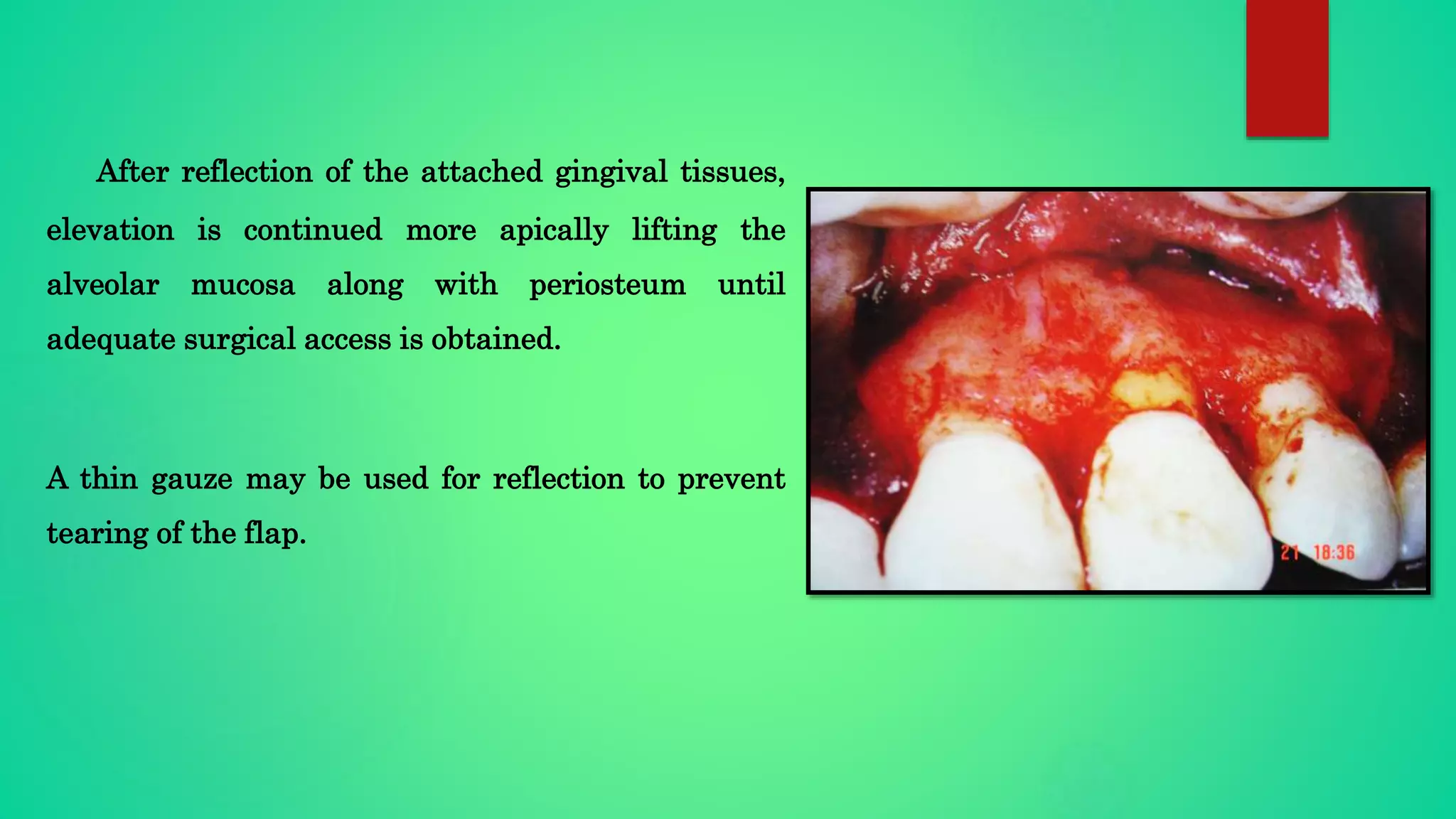
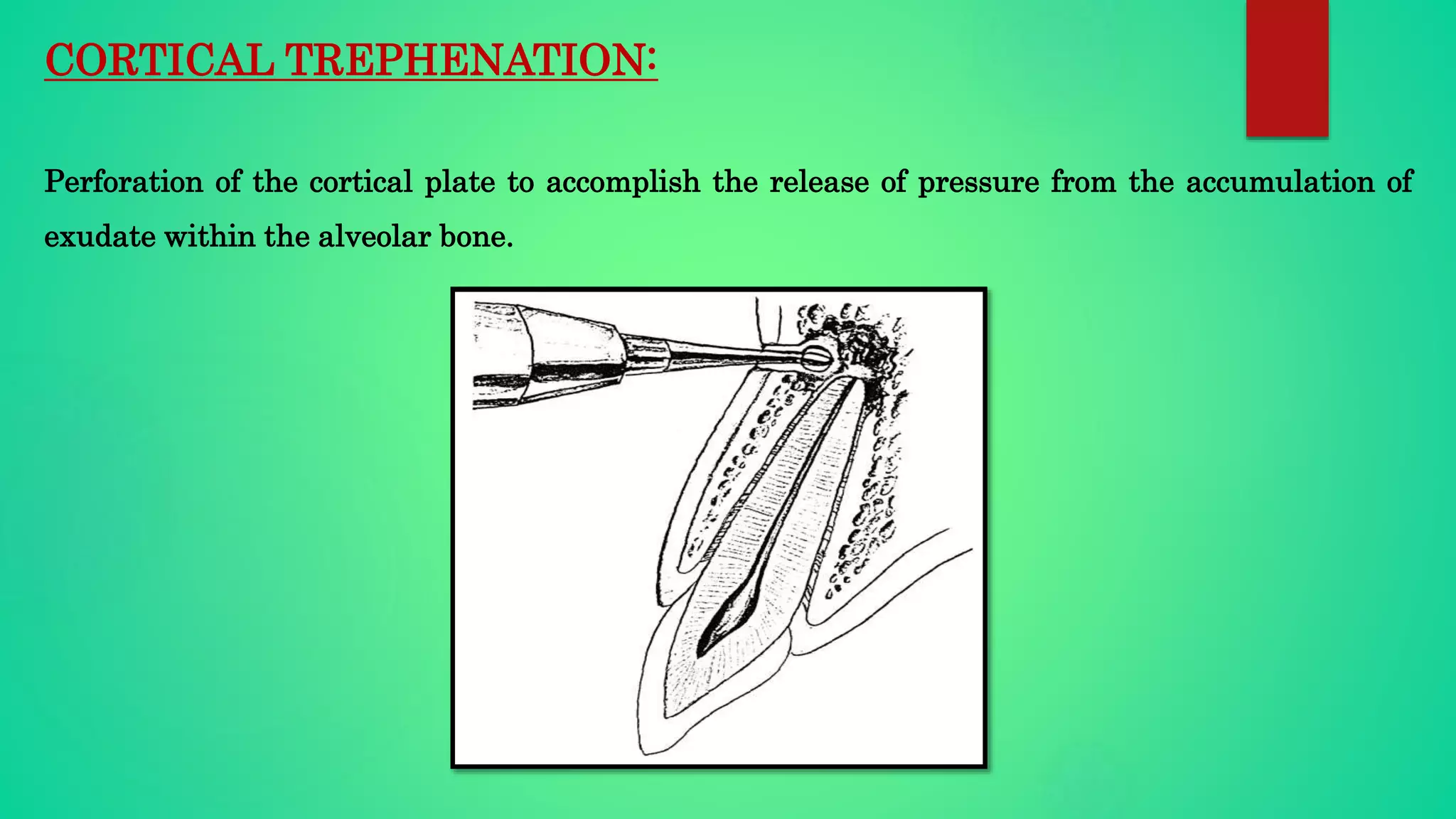
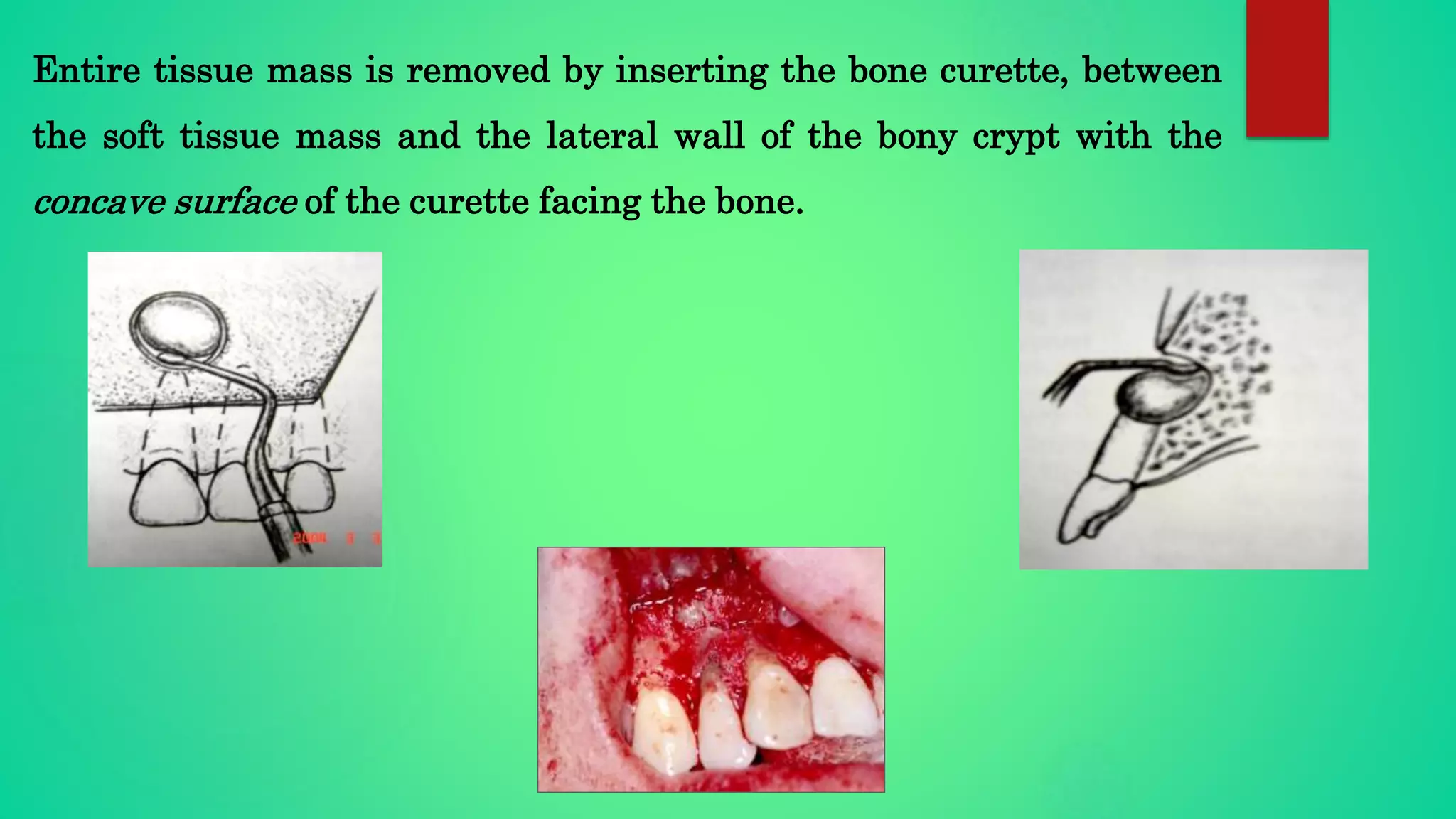
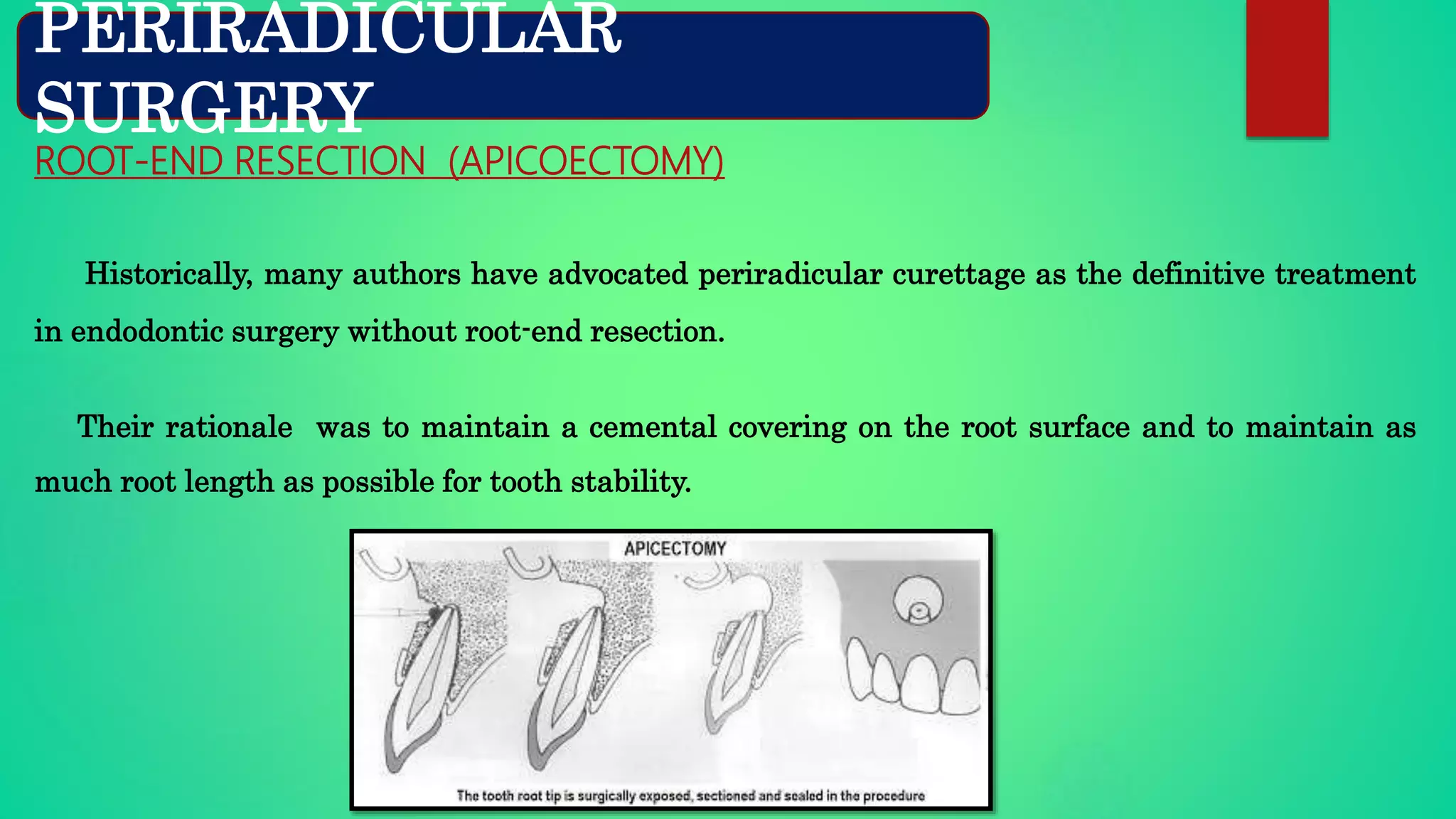
This document provides an overview of endodontic surgery. It begins with definitions and a brief history of endodontic surgery. It then discusses indications, contraindications, classifications of endodontic surgeries, and recent advances. The document covers various surgical procedures like incision and drainage, flap design, osteotomy, periradicular curettage, root-end resection, root-end preparation, and root-end filling. It provides details on techniques, principles, and advantages/disadvantages of these procedures. Overall, the document serves as a comprehensive guide to endodontic surgery.




































































![Traditional Endodontic Surgery Versus Modern Technique: A 5-Year Controlled Clinical Trial
Silvia Tortorici, MD,* Paolo Difalco, DDS, PhD,* Luigi Caradonna, MD,* and Stefano Tete`, MDÞ
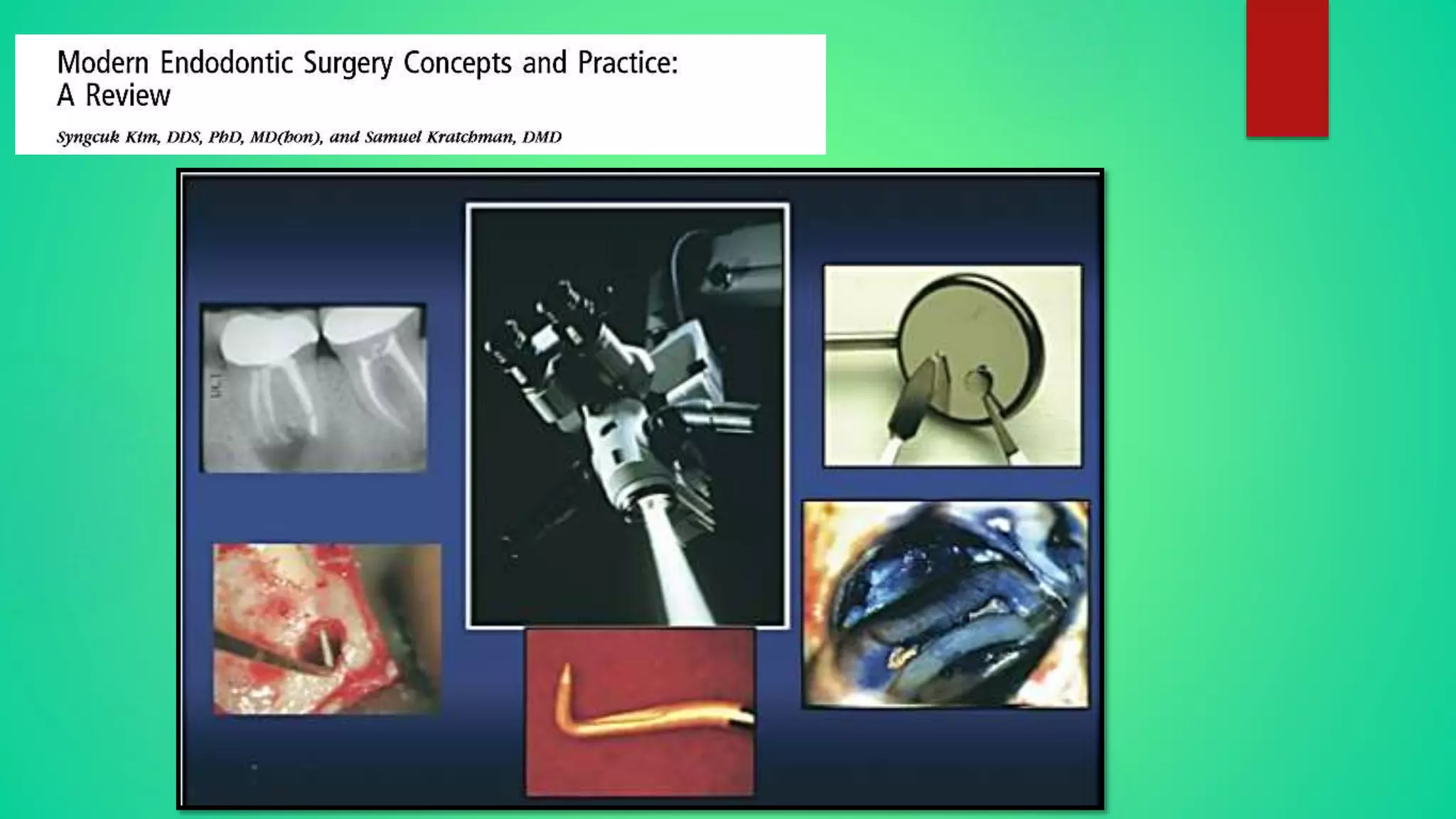
Compared traditional apicoectomy versus modern apicoectomy, method of osteotomy (type of
instruments used), type of preparation of retrograde cavity (different apicoectomy angles and
instruments used for root-end preparation), and root-end filling material used (gray mineral trioxide
aggregate or silver amalgam).
In conclusion, modern apicoectomy resulted in a probability of success more than 5 times higher (odds
ratio, 5.20 [95% confidence interval, 3.94Y6.92]; P G 0.001) compared with the traditional technique.](https://image.slidesharecdn.com/periapicalsurgeryviji-181115111345/75/Periapical-surgery-viji-90-2048.jpg)