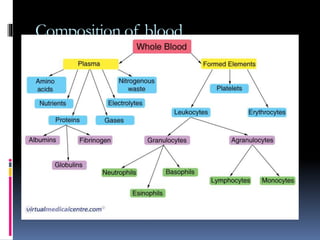
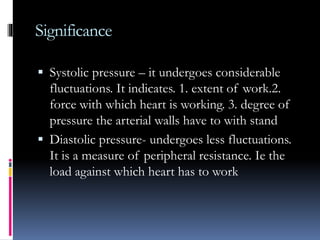
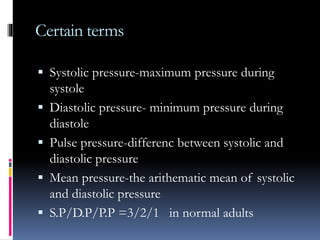
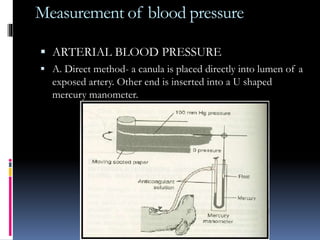
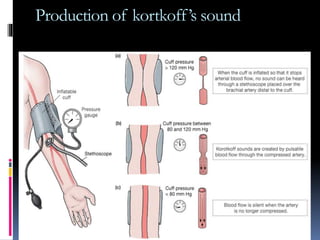
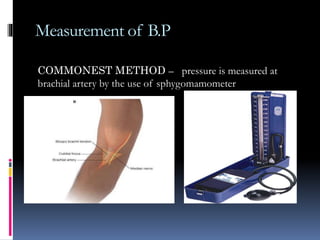
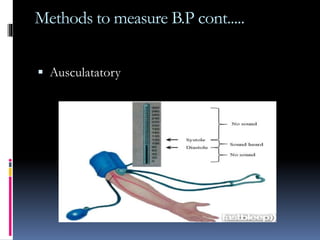
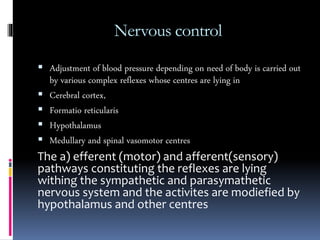
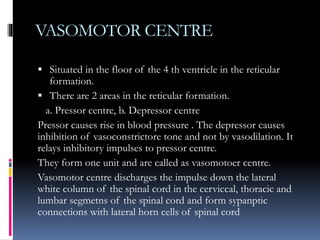
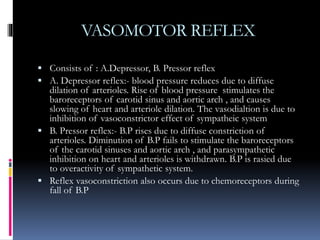
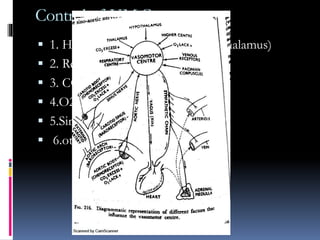
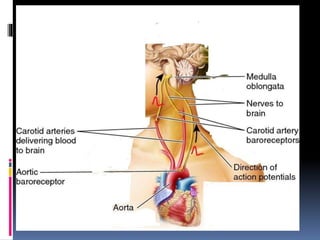
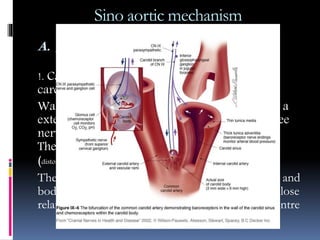
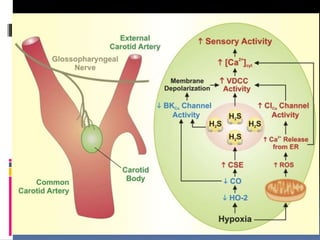
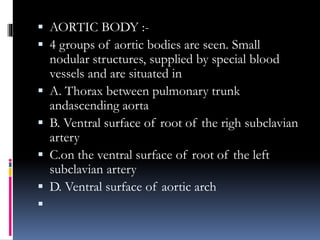
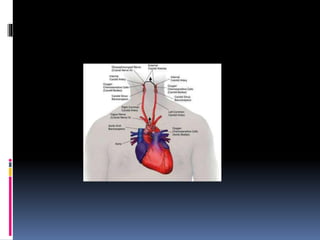
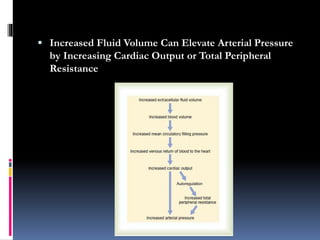
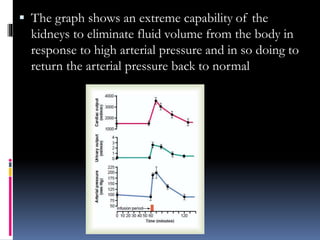
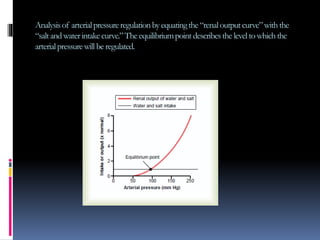
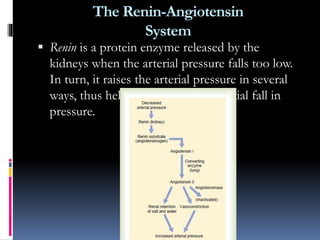
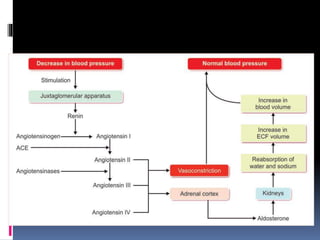
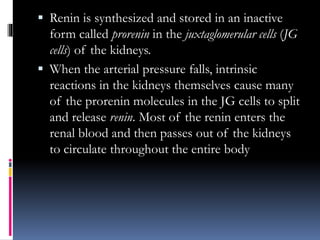
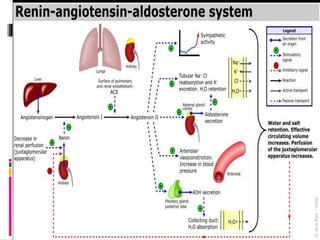
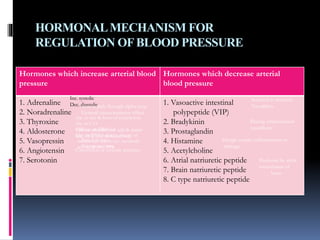
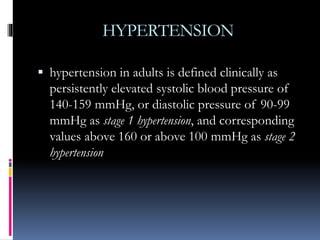
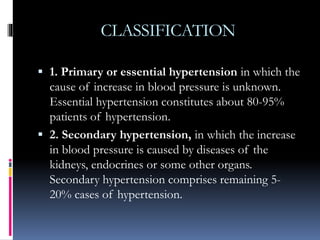
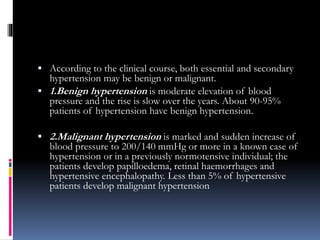
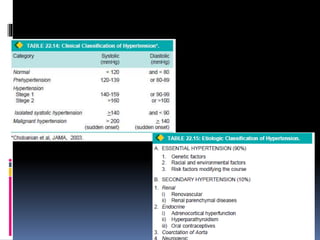
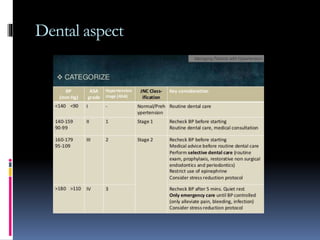
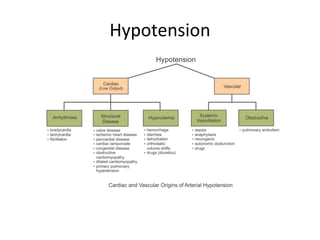
Blood pressure is regulated through several mechanisms including the nervous system, kidneys, hormones, and locally produced chemicals. The document discusses the components of blood, normal blood pressure ranges, factors controlling blood pressure such as cardiac output and peripheral resistance, and conditions such as hypertension. Measurement of blood pressure is described including the auscultatory method using Korotkoff sounds. Mechanisms for regulating blood pressure involve baroreceptors, chemoreceptors, the renin-angiotensin system, and renal control of fluid balance and salt.