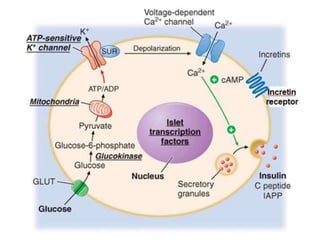
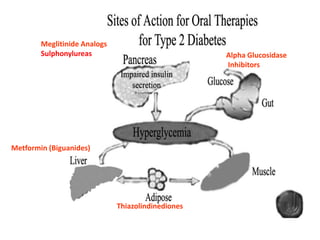
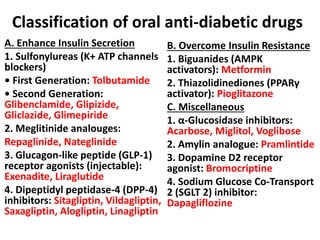
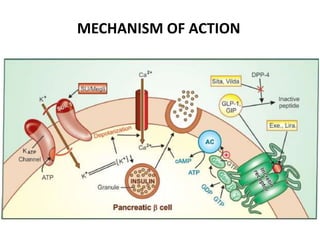
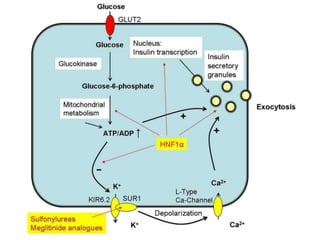
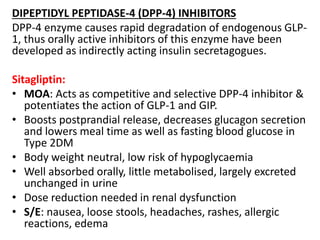
This document provides information on the classification and mechanisms of action of various oral anti-diabetic drugs. It discusses drugs that enhance insulin secretion like sulfonylureas and meglitinides, drugs that overcome insulin resistance like metformin and thiazolidinediones, and other drugs like alpha-glucosidase inhibitors. For each class, it describes the specific drugs, their mechanisms of action involving pathways and targets like K+ channels, AMPK activation and PPARγ agonism, pharmacokinetics, indications, and adverse effects.