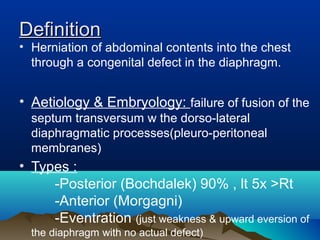
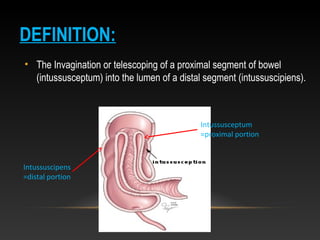
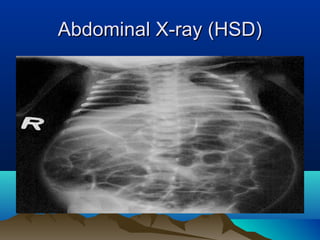
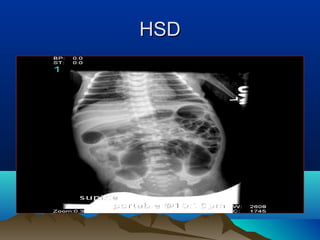
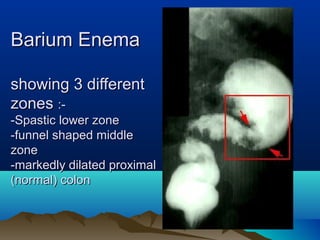
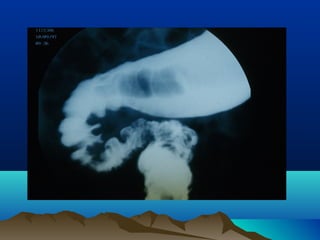
1. The document provides an overview of common pediatric surgical conditions, including congenital diaphragmatic hernia, esophageal atresia with tracheoesophageal fistula, congenital hypertrophic pyloric stenosis, intussusception, Meckel's diverticulum, Hirschsprung disease, and anorectal malformations.
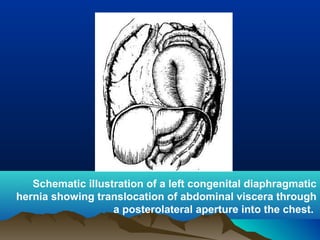
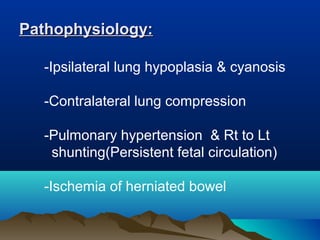
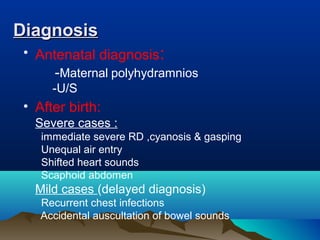
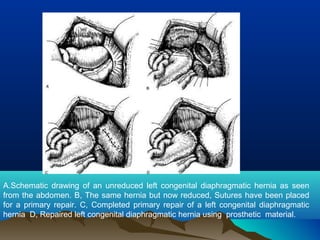
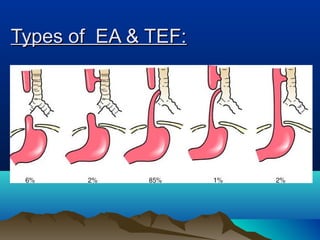
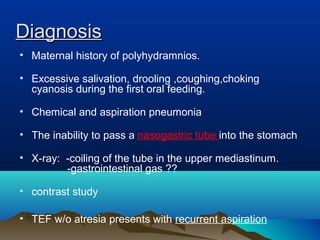
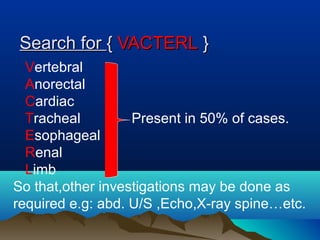
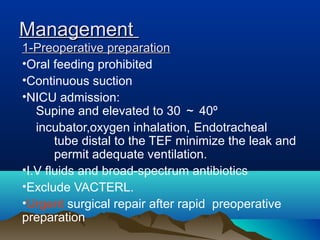
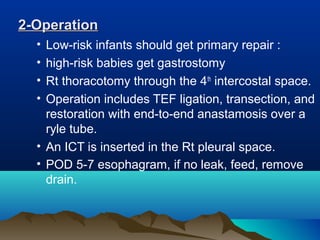
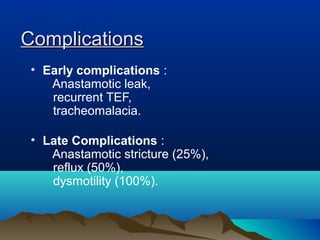
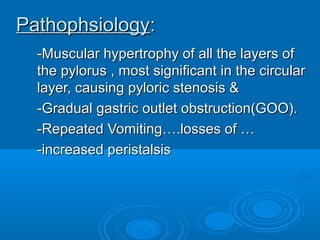
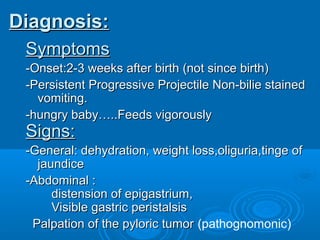
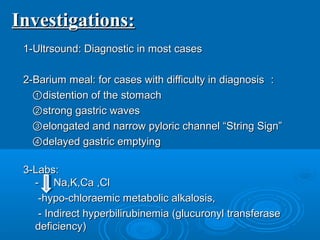
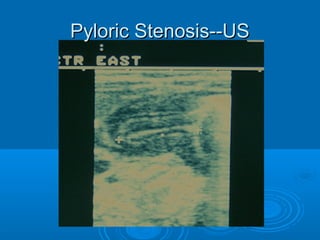
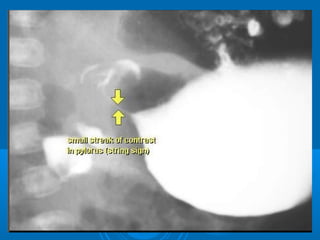
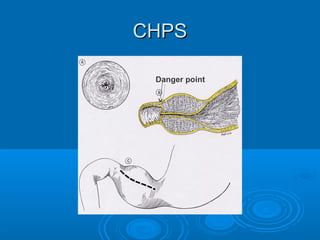
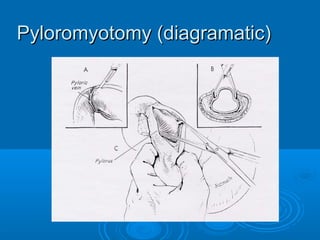
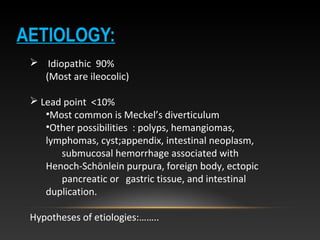
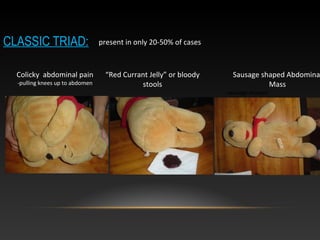
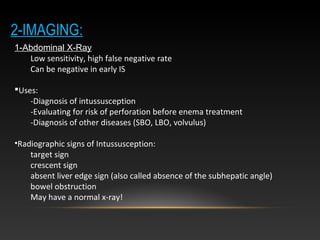
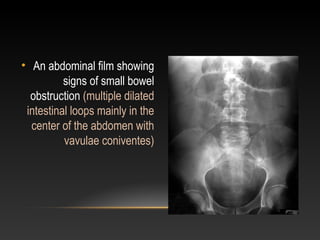
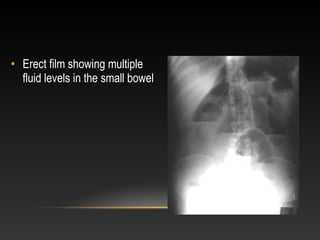
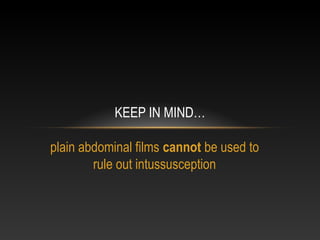
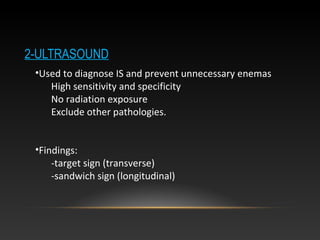
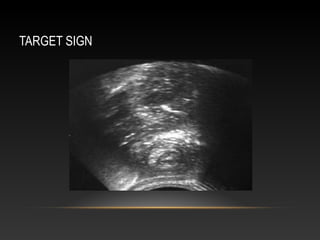
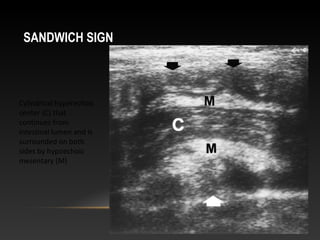
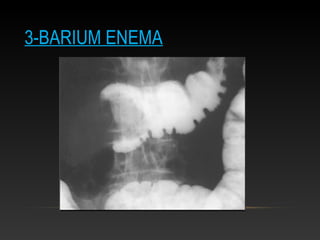
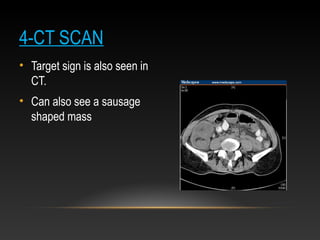
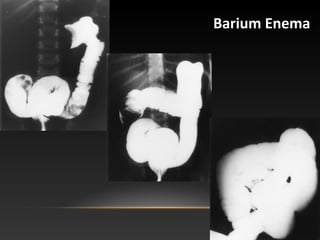
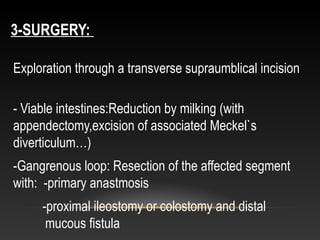
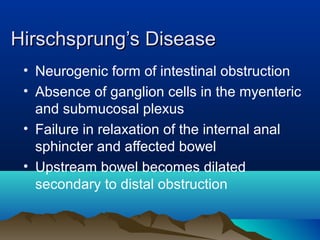
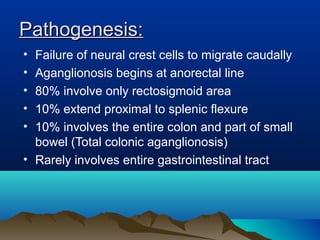
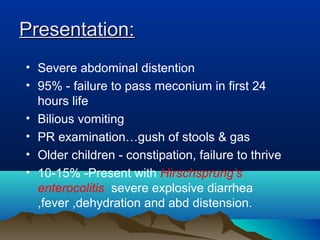
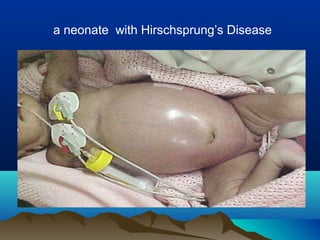
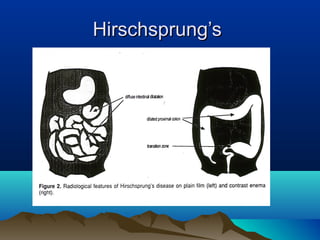
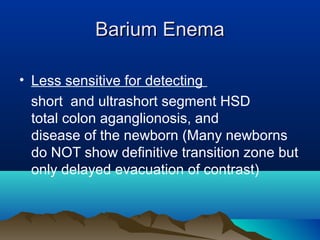
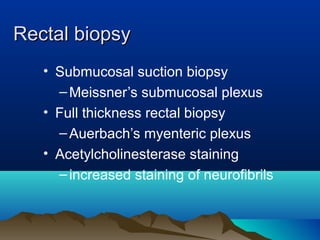
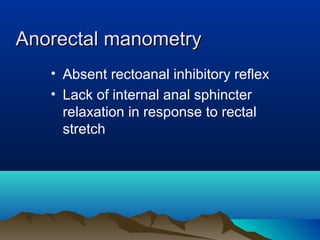
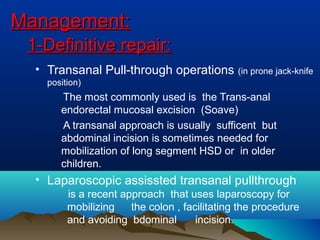
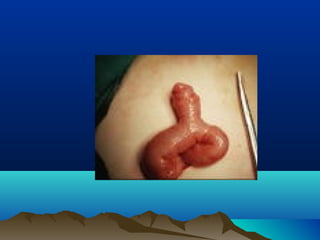
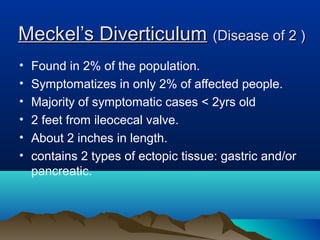
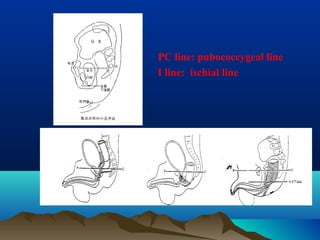
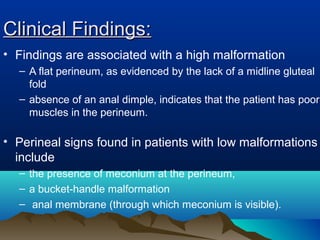
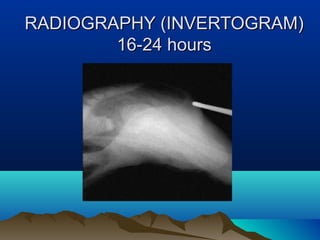
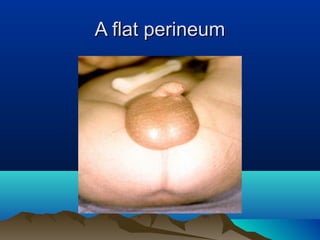
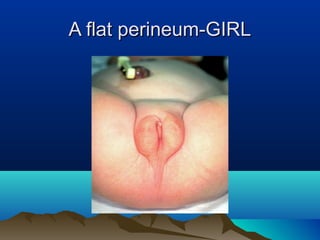
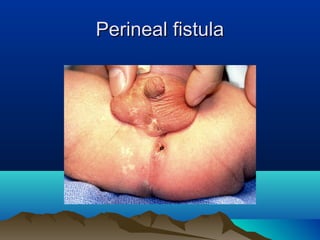
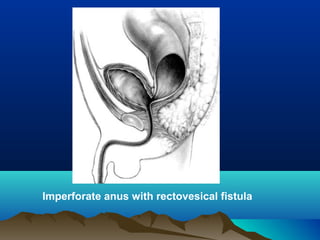
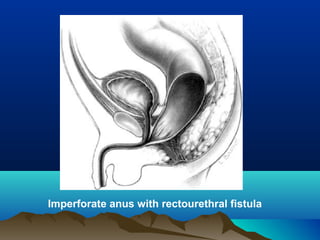
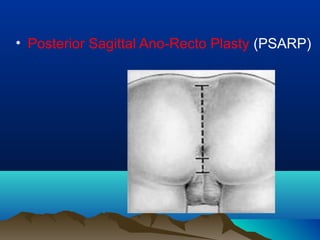
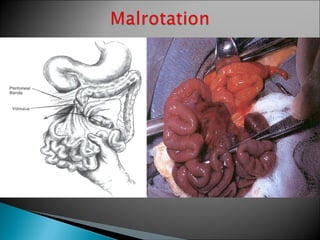
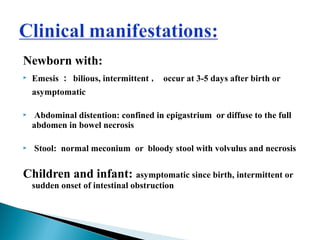
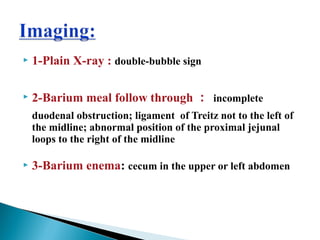
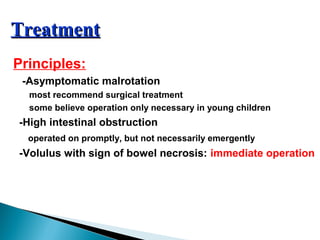
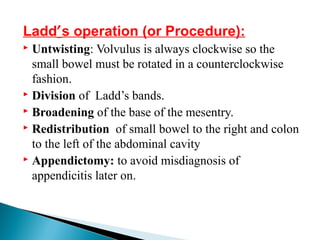
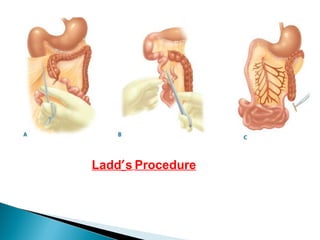
2. It describes the definition, etiology, pathophysiology, clinical presentation, diagnostic workup, and management of each condition. Diagrams and images are provided to illustrate key aspects.
3. The review is intended for 6th year medical students to familiarize them with important pediatric surgical topics.