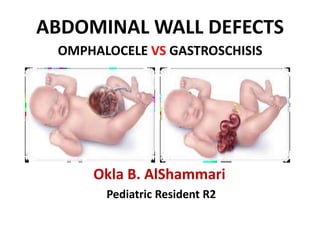
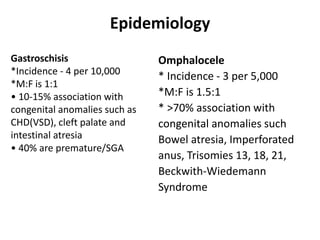
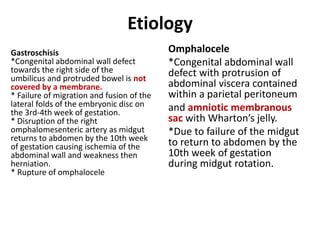
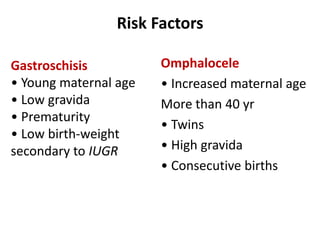
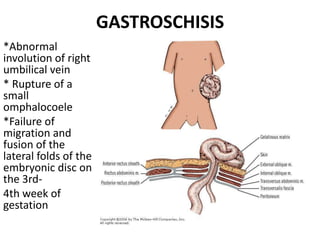
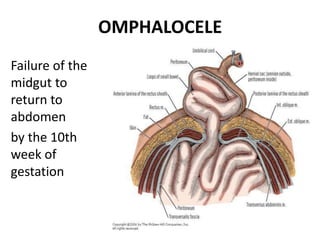
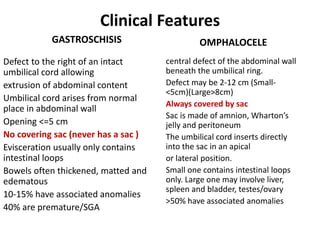
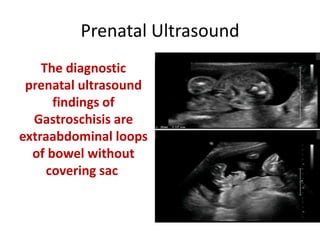
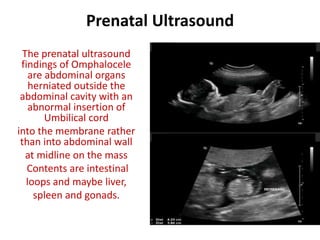
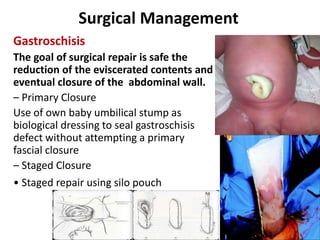
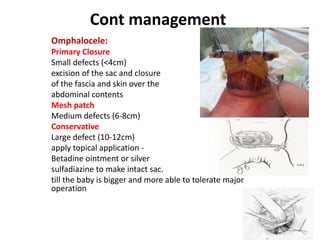
This document provides information on abdominal wall defects, specifically omphalocele and gastroschisis. It discusses the epidemiology, etiology, clinical features, diagnosis, management, and prognosis of each condition. Omphalocele is caused by failure of the midgut to return to the abdomen during development. It presents as abdominal organs herniated within a sac. Gastroschisis is caused by failure of abdominal wall closure and presents as bowel protruding through an abdominal wall defect without a sac. Management may include prenatal monitoring, temporary covering of exposed organs, surgery to repair the defect, and treatment of any associated anomalies or complications. Outcomes depend on the severity of each case and presence of other birth defects