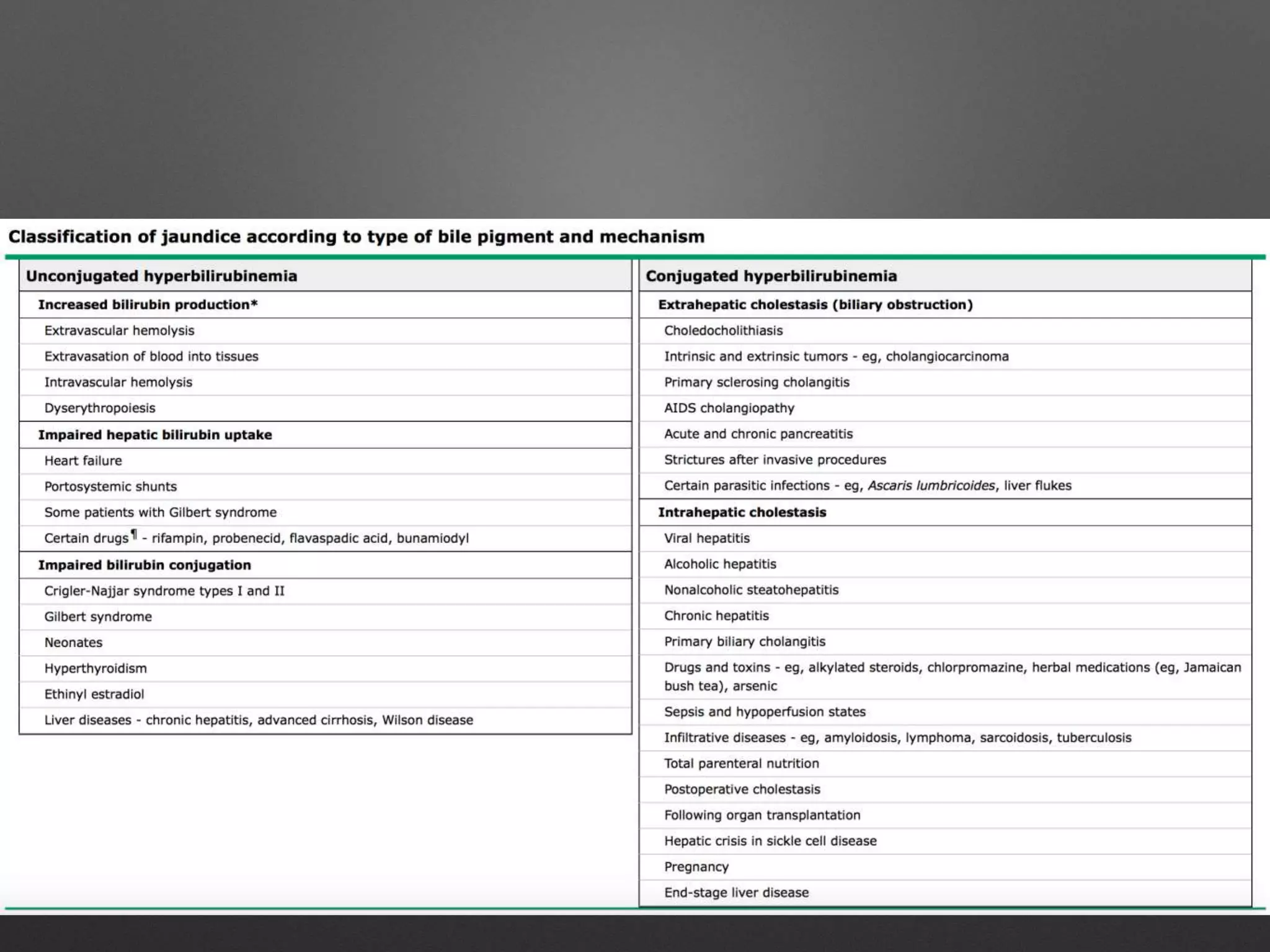
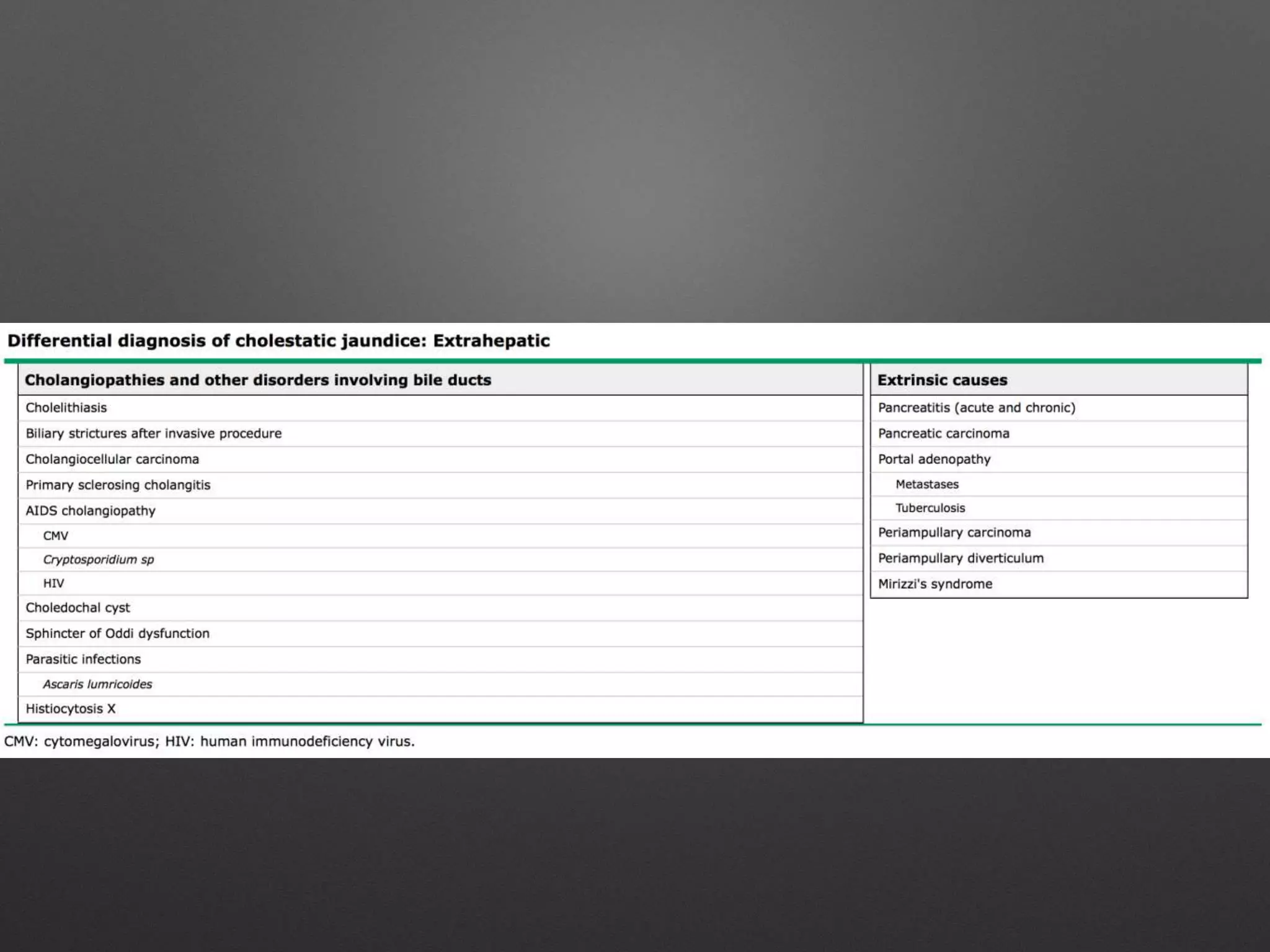
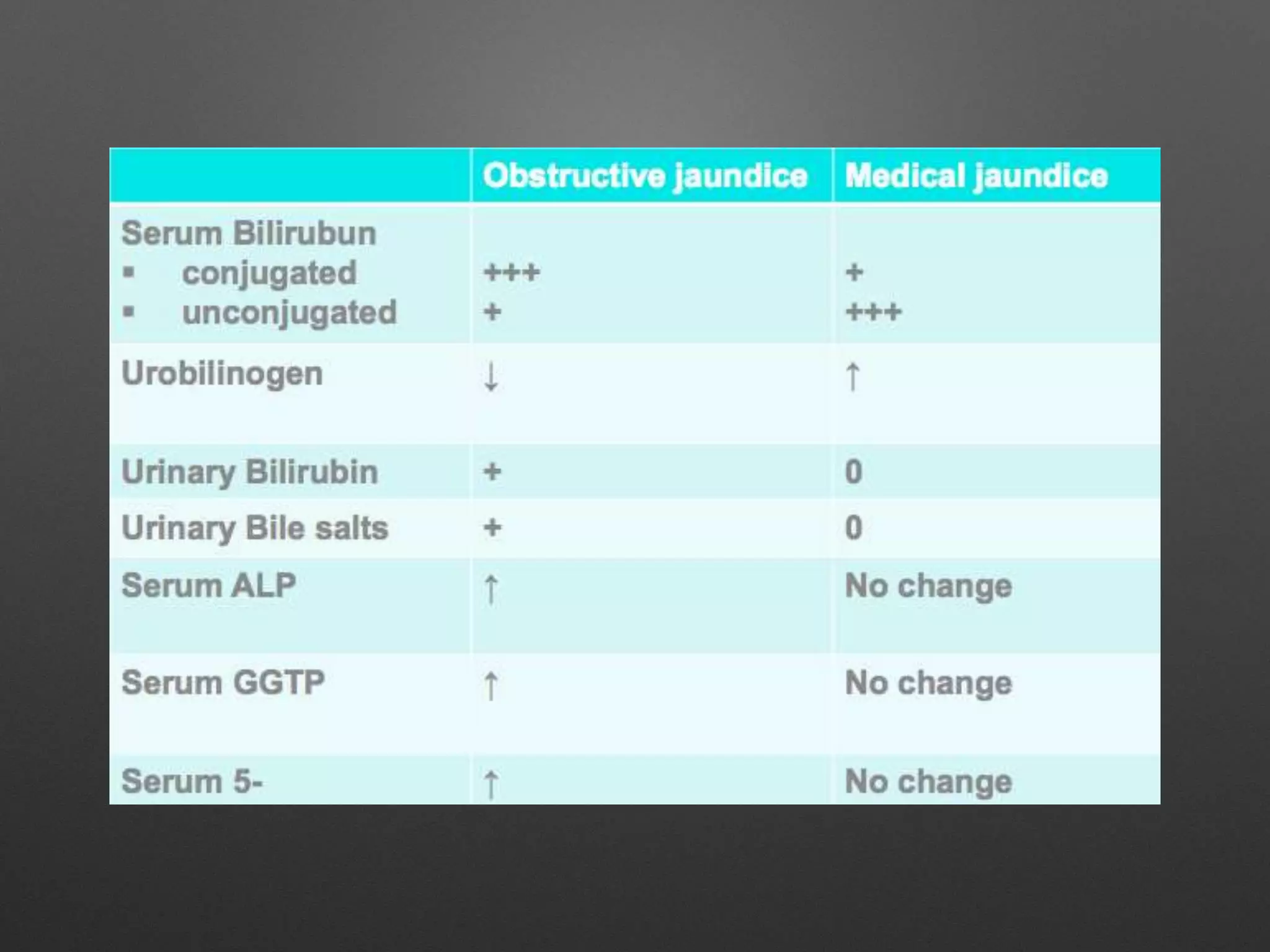
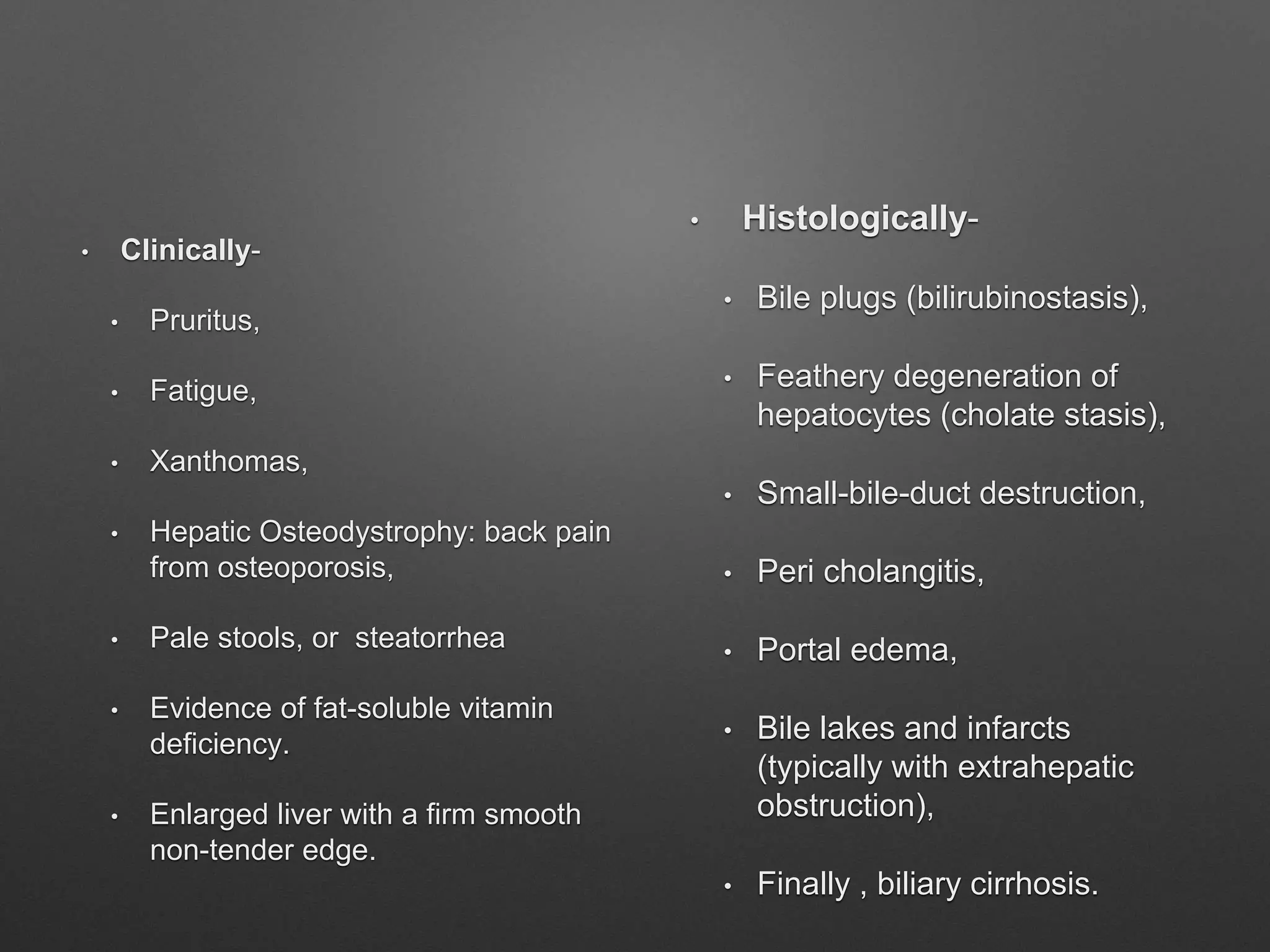
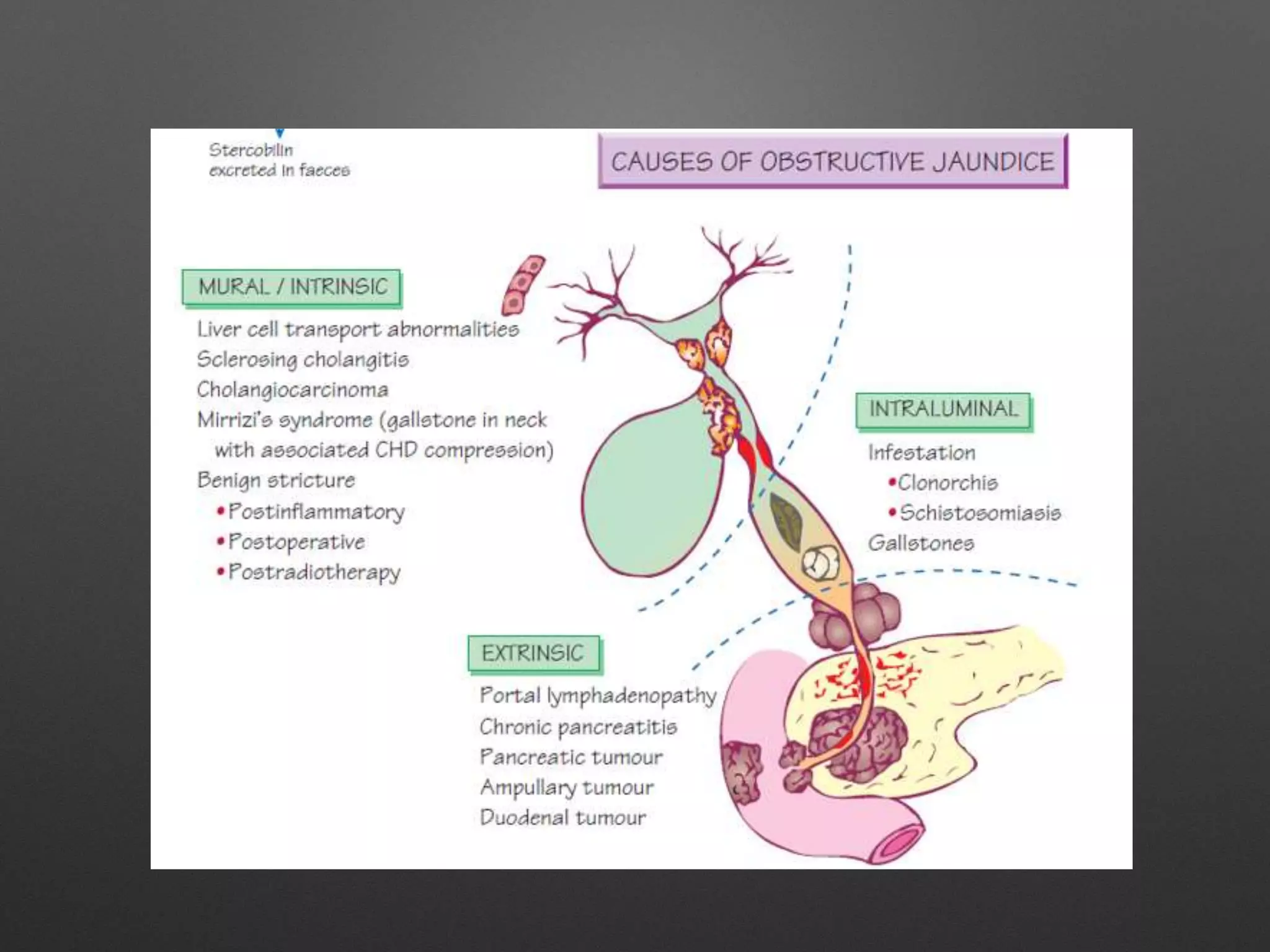
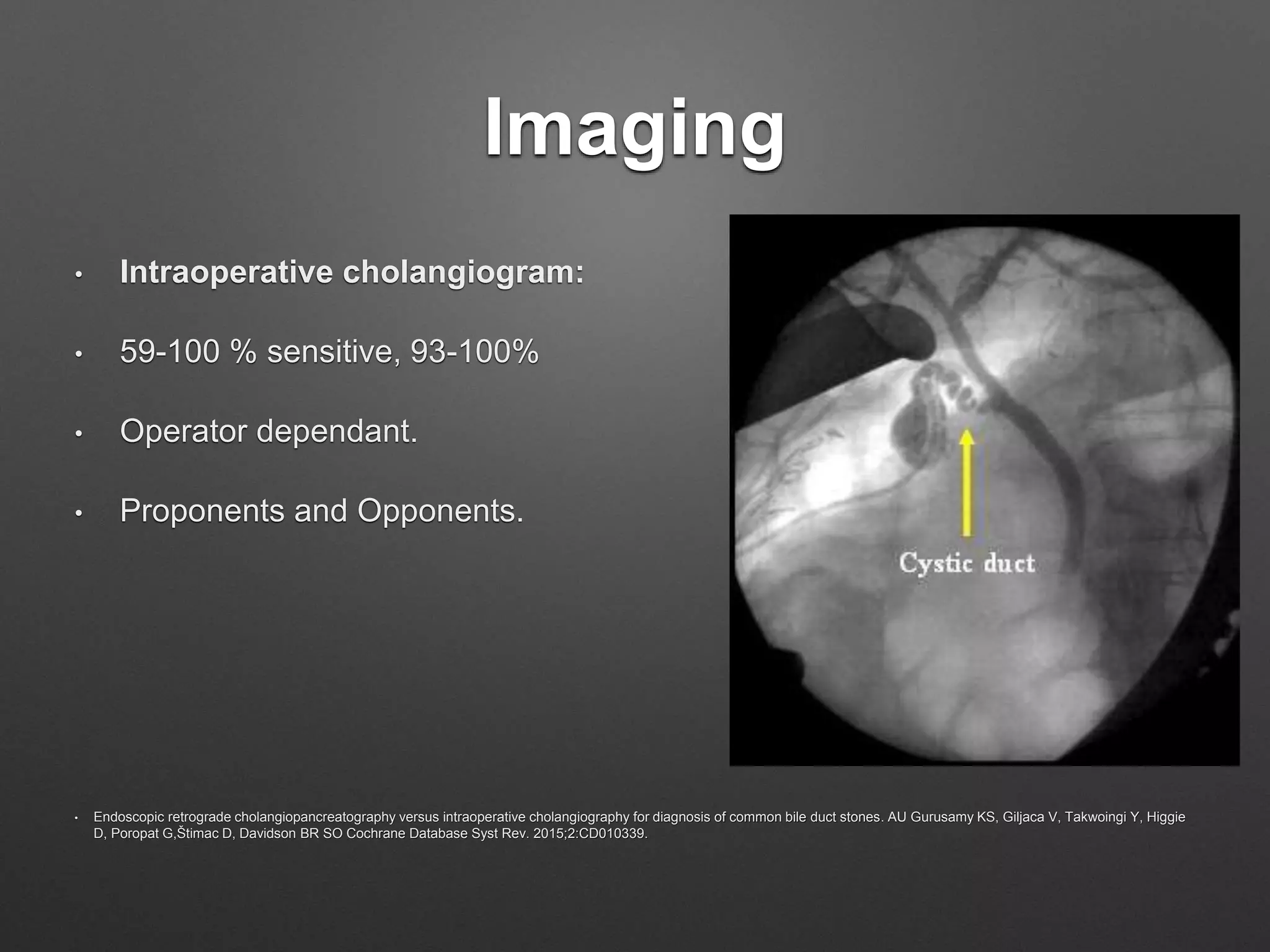
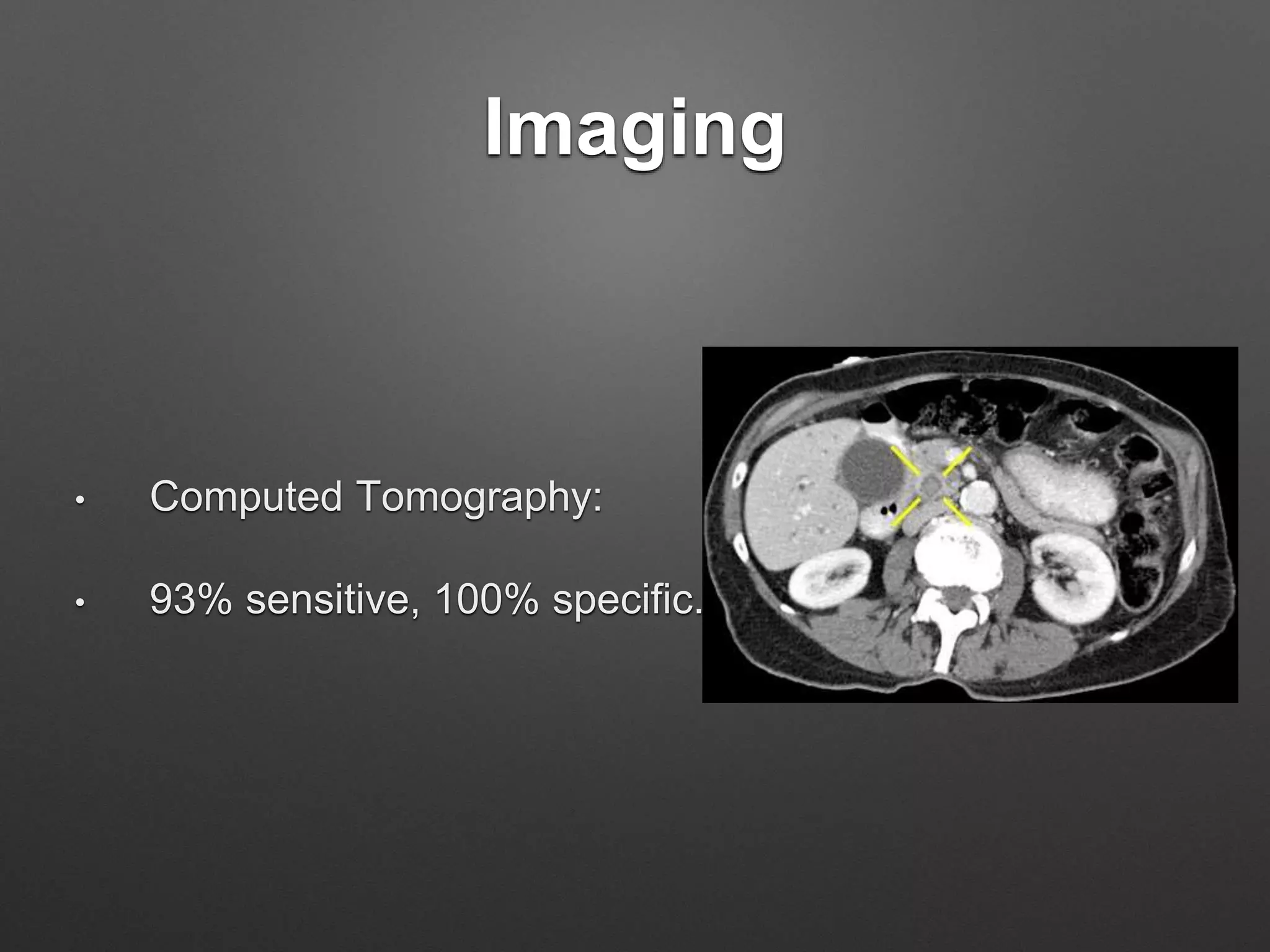
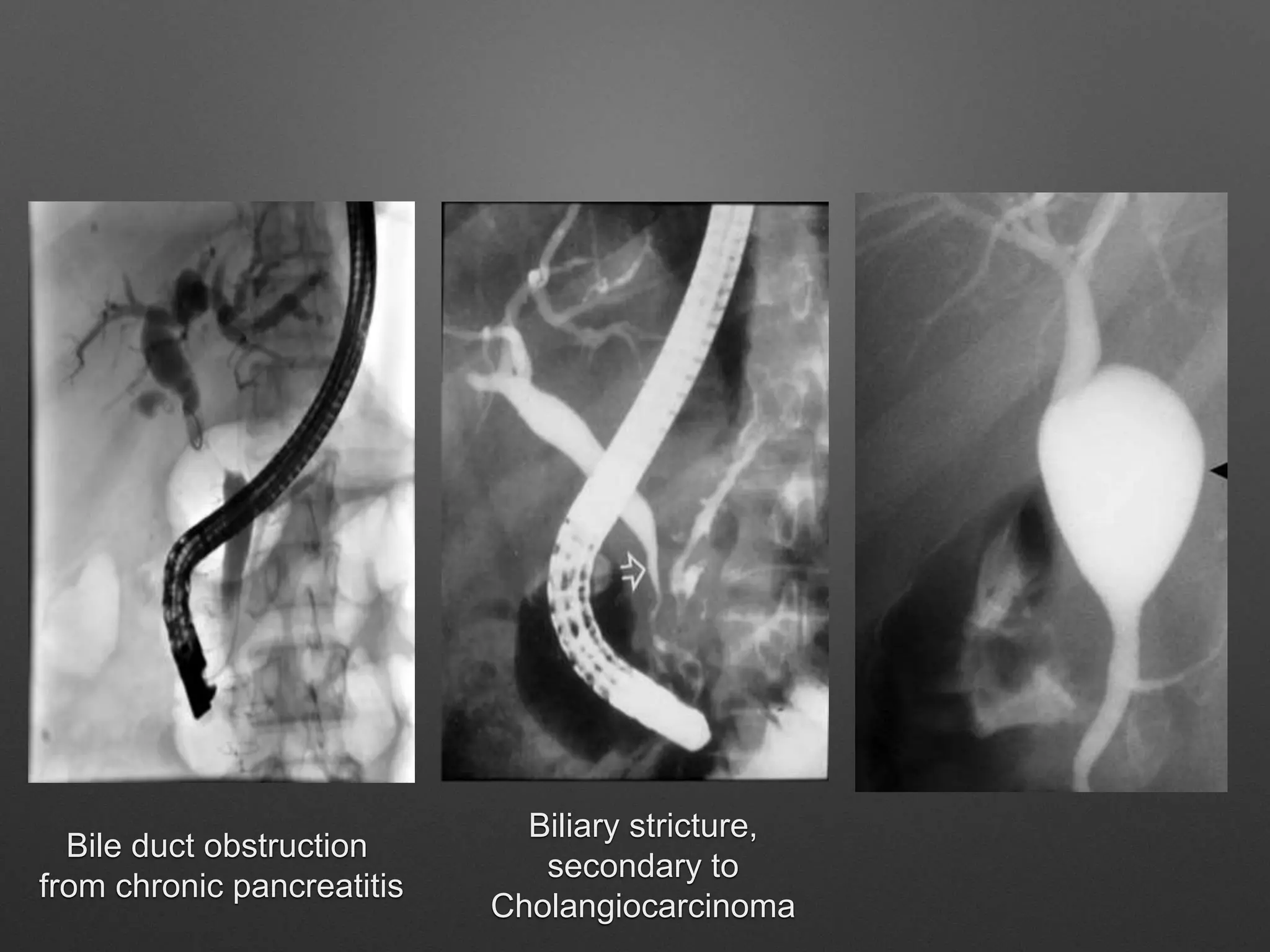
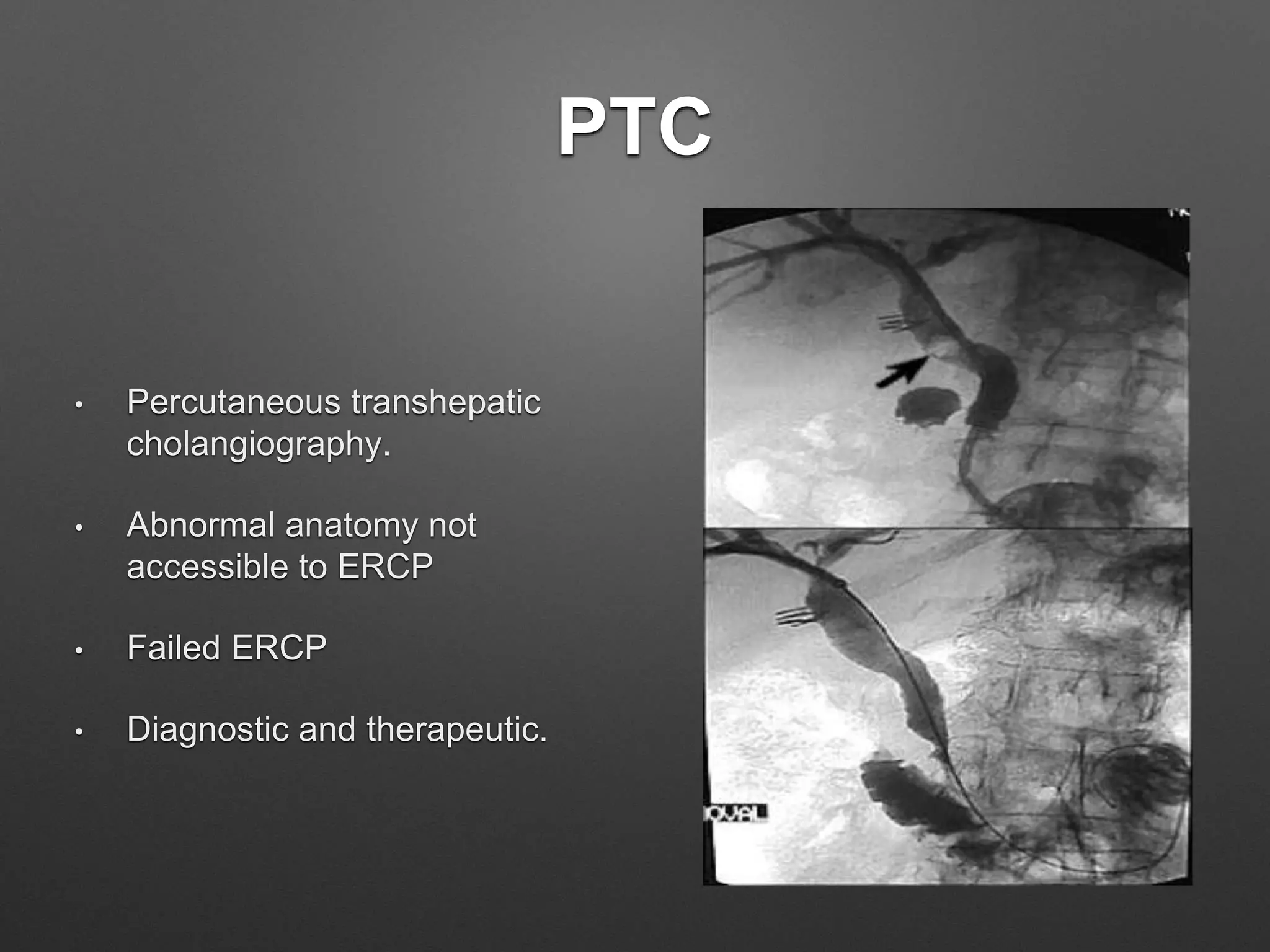
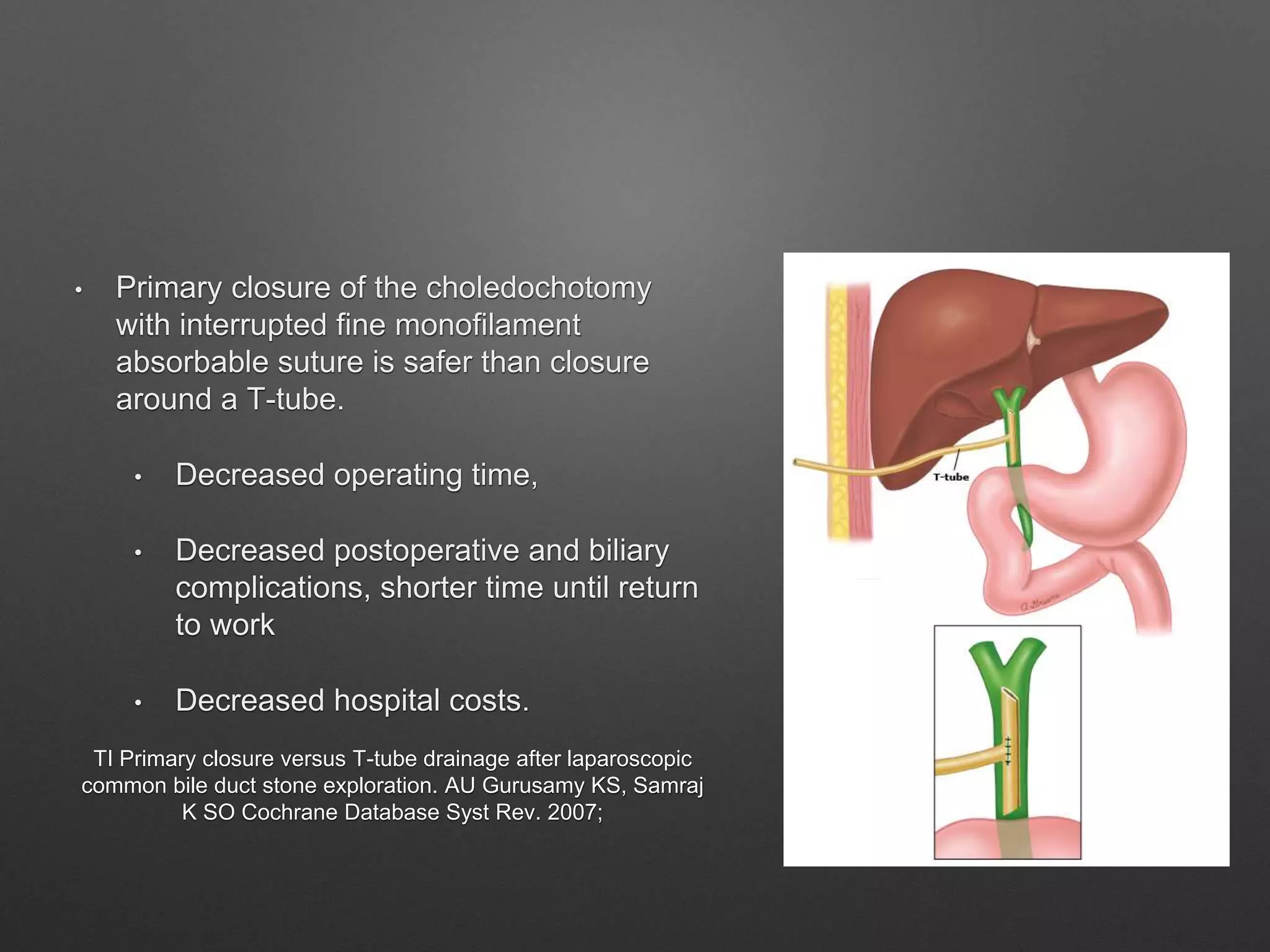
This document provides an overview of the management of obstructive jaundice. It begins with definitions and classifications of jaundice. Obstructive jaundice can be intrahepatic or extrahepatic in origin. Common causes of intrahepatic cholestasis include viral hepatitis, alcoholic hepatitis, and drug toxicity. Extrahepatic obstructions are often due to choledocholithiasis (gallstones in the common bile duct), tumors, or strictures. Diagnostic imaging includes ultrasound, MRCP, ERCP, and intraoperative cholangiography. Treatment depends on whether the obstruction is pre-operative or discovered during cholecystectomy, and may involve ERCP, laparoscopic or open CBD exploration, or