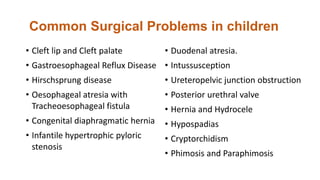
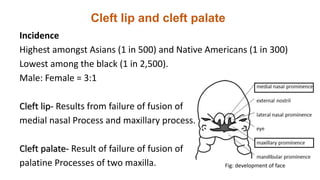
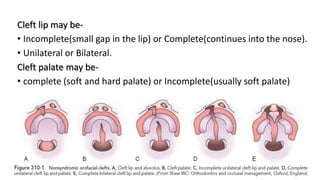
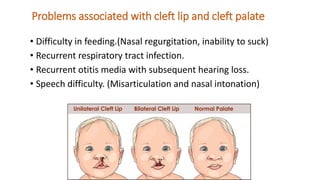
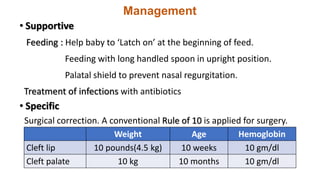
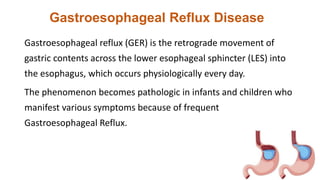
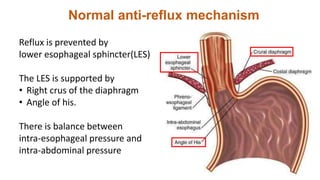
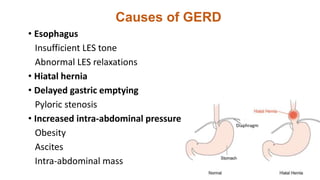
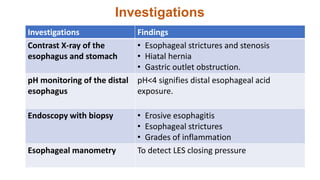
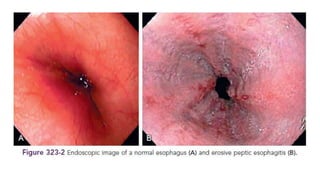
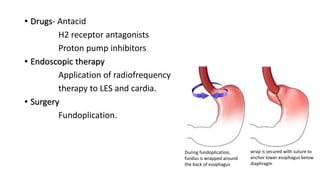
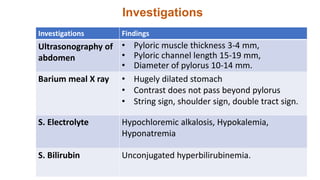
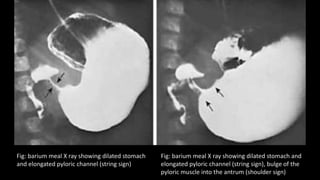
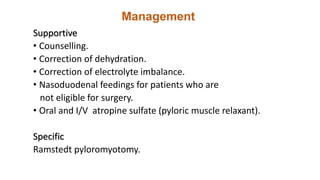
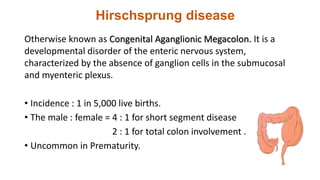
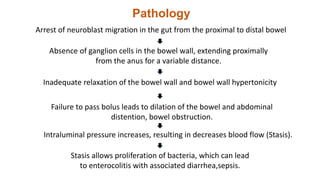
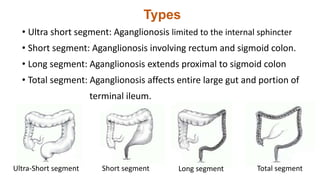
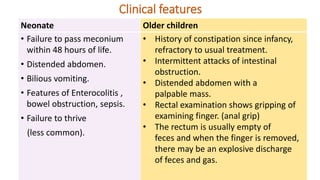
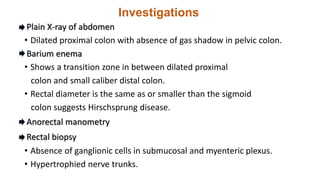
This document summarizes several common surgical problems in children. It discusses conditions like cleft lip and palate, gastroesophageal reflux disease, infantile hypertrophic pyloric stenosis, and Hirschsprung disease. For each condition, it provides information on incidence, clinical features, investigations, and management. The goal is to provide pediatricians with sound knowledge of these common pediatric surgical issues.