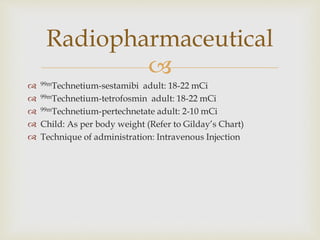
The document provides an overview of the parathyroid glands' location, size, and role in hyperparathyroidism management through nuclear medicine. It outlines procedures for non-invasive identification of hyperfunctioning parathyroid tissues, including patient preparations and techniques for scintigraphy. Additionally, it emphasizes the importance of imaging protocols and includes precautions for pregnant and nursing patients.










![Washout Procedure
Static ANT/POST 20 mins after injection of Tetrofosmin
SPECT
If needed
Pinhole
Static Tetrofosmin 60 mins after inject
Pinhole
If needed
SPECT
Static Tetrofosmin delayed 2 hours after inject
SPECT
If needed
Pinhole
[Delayed 3 hours after inject if necessary]
Static
Pinhole
If needed
SPECT](https://image.slidesharecdn.com/parathyroidscan-140929214754-phpapp01/85/Parathyroid-Scan-12-320.jpg)
![Subtraction Procedure
Static ANT/POST 20 mins after injection of Tc99m
SPECT
If needed
Pinhole
Pinhole Tetrofosmin 60 mins after inject
Static
If needed
SPECT
Static Tetrofosmin delayed 2 hours after inject
SPECT
If needed
Pinhole
[Delayed 3 hours after inject if necessary]
Pinhole
Static
SPECT
If needed](https://image.slidesharecdn.com/parathyroidscan-140929214754-phpapp01/85/Parathyroid-Scan-13-320.jpg)








