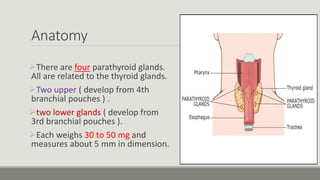
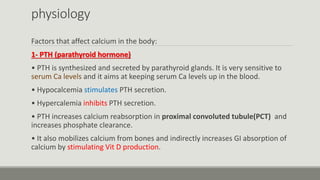
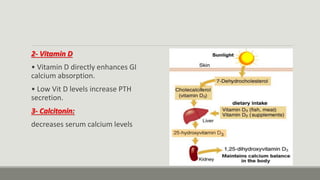
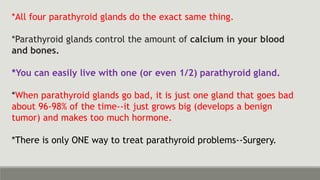
The parathyroid glands regulate calcium levels in the blood and bones. There are usually four parathyroid glands located near the thyroid gland. The parathyroid glands secrete parathyroid hormone (PTH) which increases blood calcium levels when low by promoting bone resorption and renal reabsorption of calcium. Primary hyperparathyroidism occurs when one parathyroid gland enlarges and overproduces PTH, commonly caused by a benign tumor in the gland. Surgical removal of the enlarged gland is usually curative for primary hyperparathyroidism.