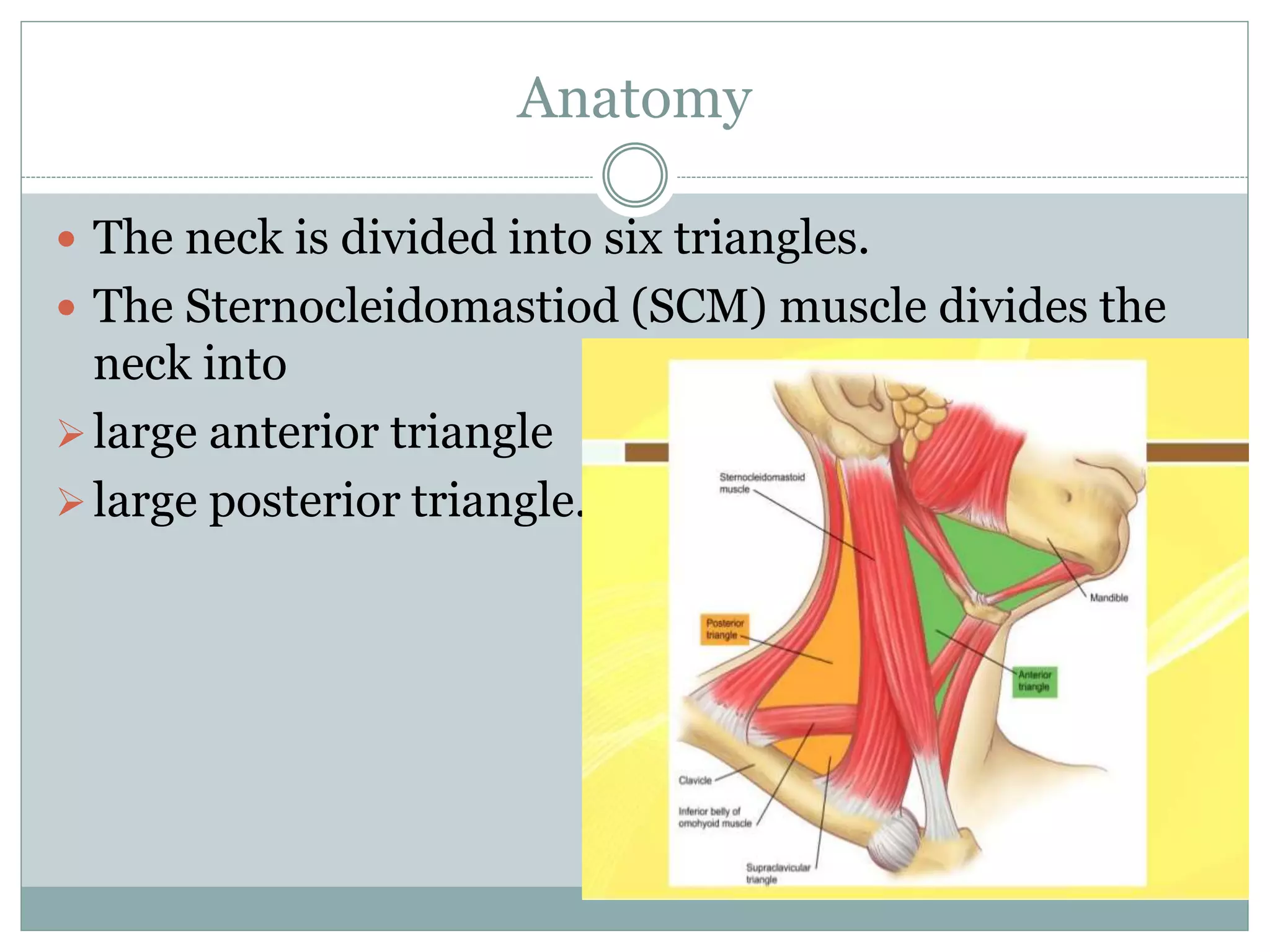
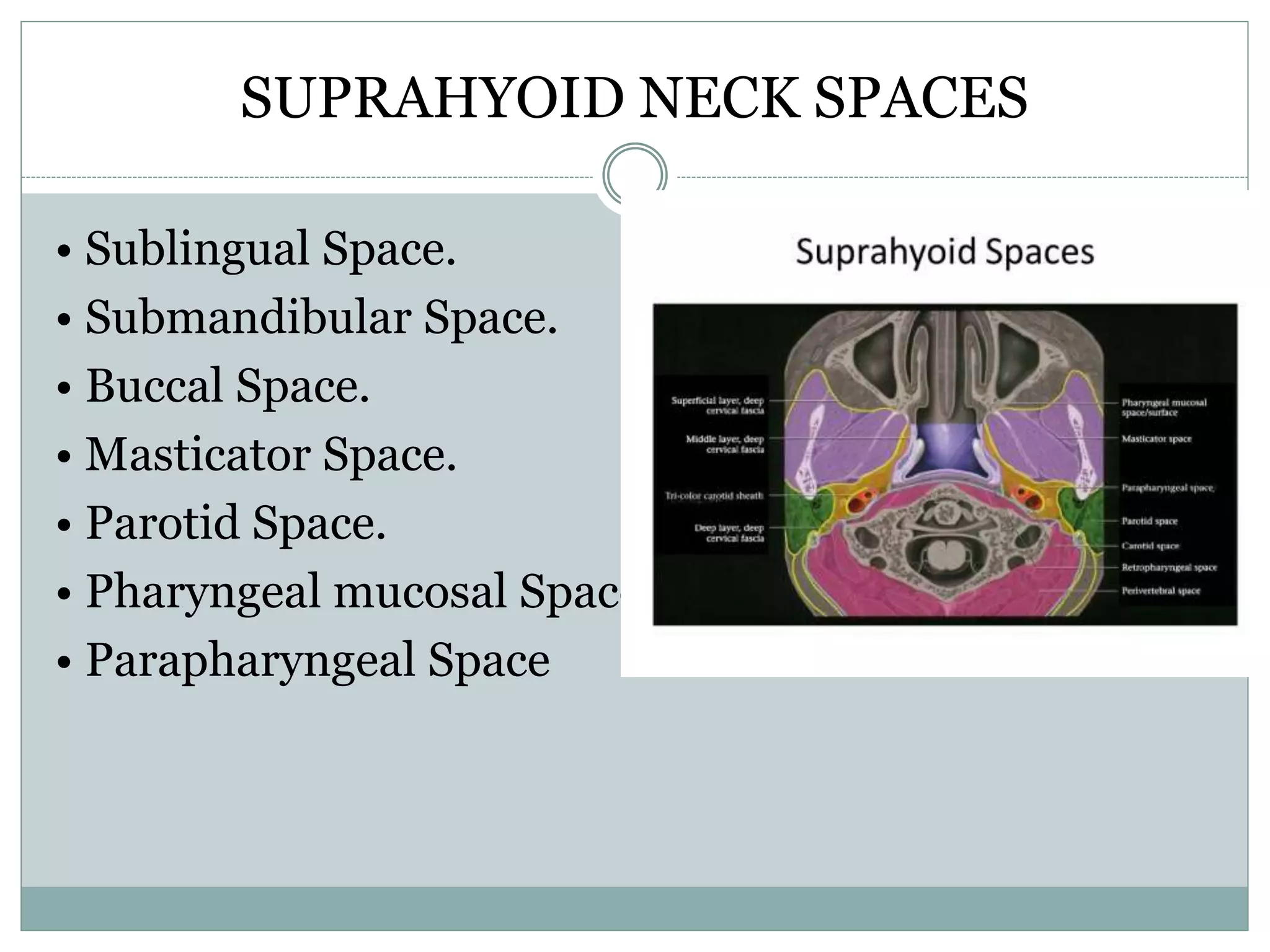
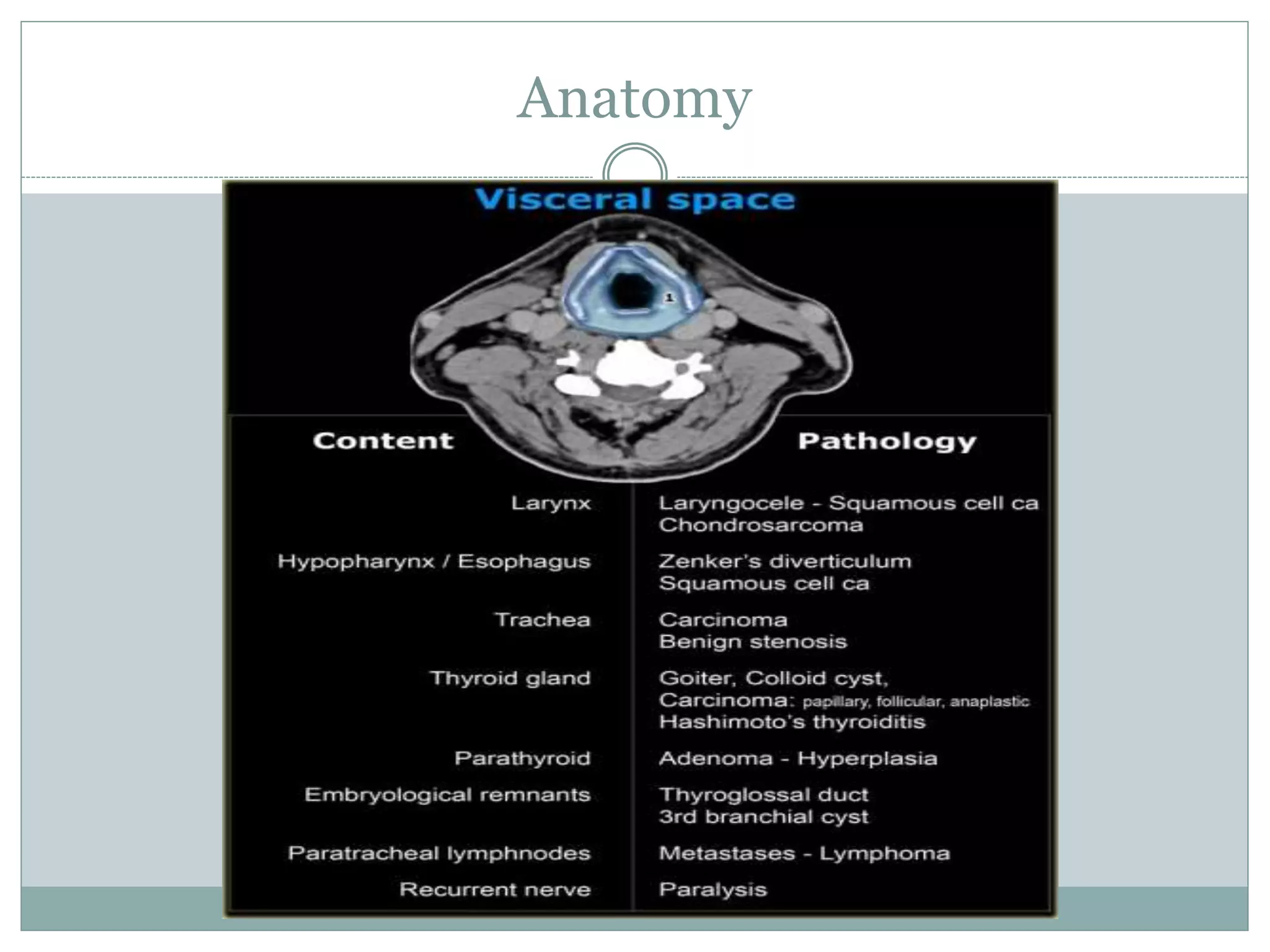
CT imaging of the neck provides detailed anatomical information and is useful for evaluating neck masses, lymphadenopathy, thyroid diseases and trauma. The neck is divided into triangles and spaces which radiologists use to characterize abnormalities. CT protocols involve intravenous contrast administration and thin slices through the neck. MRI is also used and has advantages over CT such as better soft tissue contrast without radiation, though CT remains superior for assessing bone.