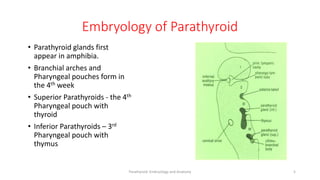
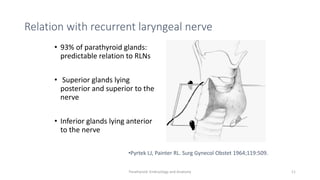
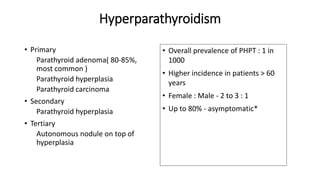
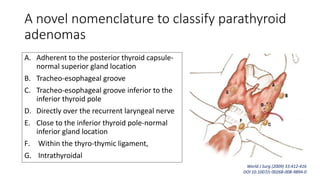
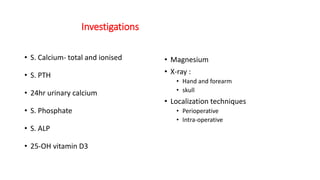
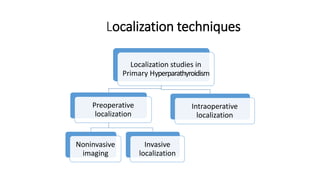
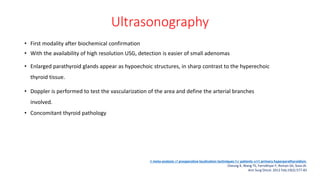
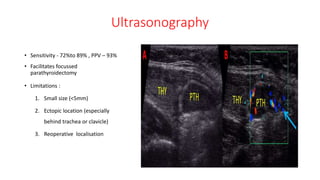
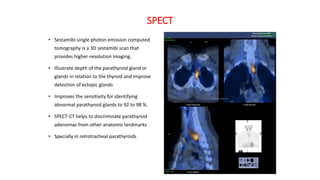
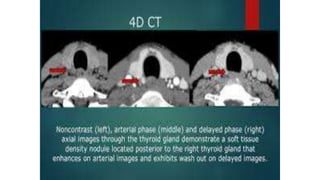
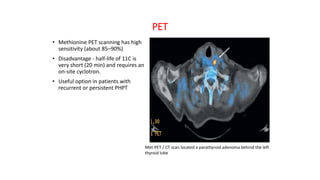
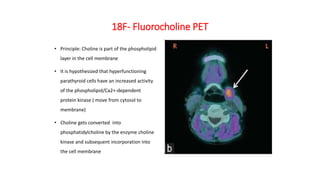
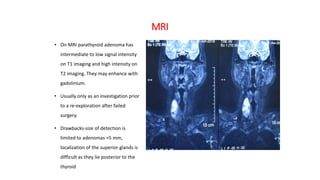
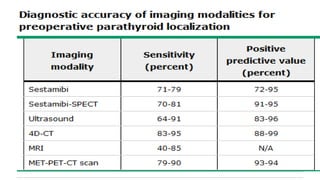
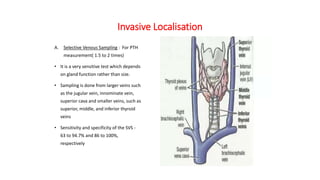
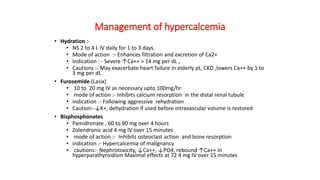
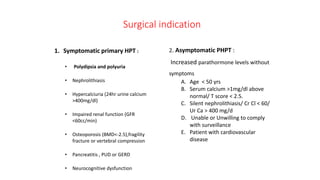
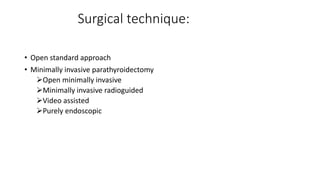
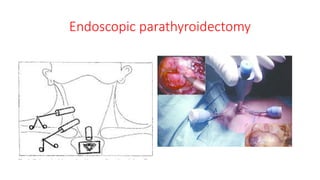
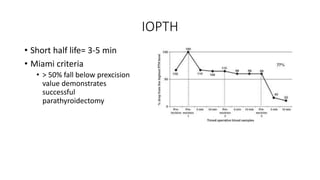
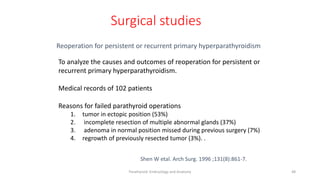
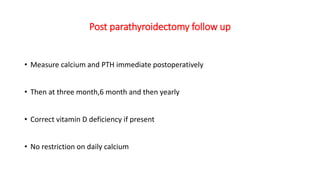
This document discusses the approach for suspected parathyroid adenoma. It begins with a brief historical overview of discoveries related to the parathyroid glands and their relationship to calcium metabolism. It then covers the embryology, anatomy, characteristics and vascular supply of the parathyroid glands. The document discusses various localization techniques used preoperatively including ultrasound, scintigraphy, SPECT, CT and MRI. It also discusses invasive techniques. Surgical indications and various surgical techniques for parathyroidectomy are outlined including open, minimally invasive and endoscopic approaches. The role of intraoperative PTH monitoring is also summarized.

![A total of 196 patients met inclusion criteria with an overall median follow-up time of
9.2 years IQR (interquartile range) [5.4-10.9 years].](https://image.slidesharecdn.com/presentationadenoma1-210217163212/85/parathyroid-adenoma-50-320.jpg)