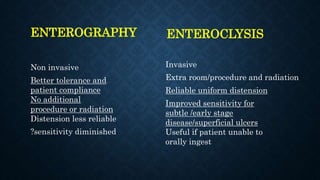
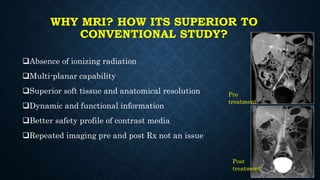
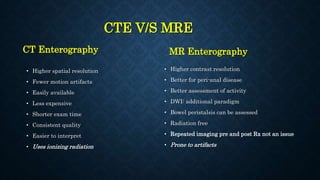
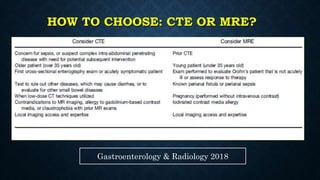
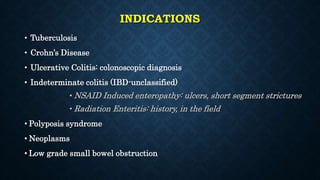
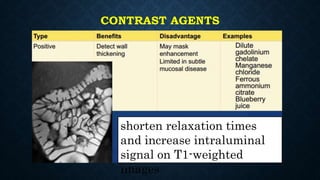
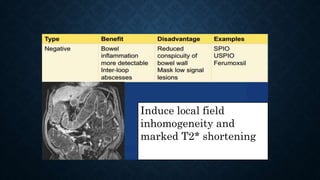
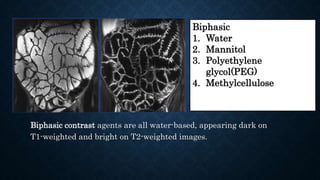
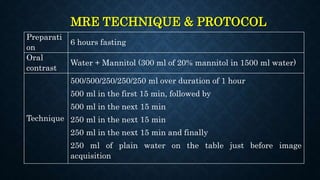
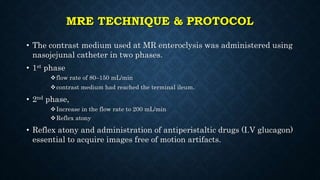
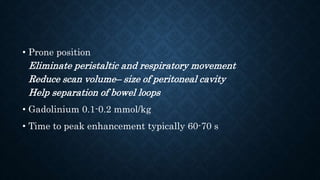
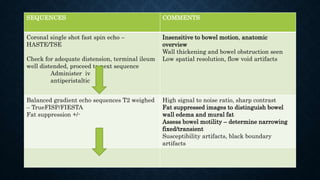
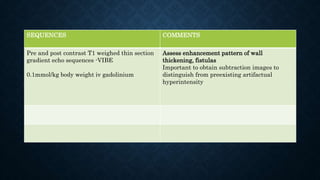
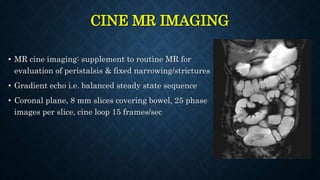
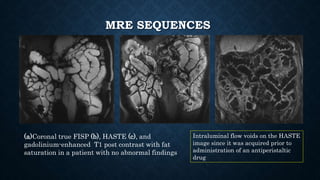
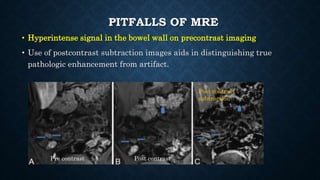
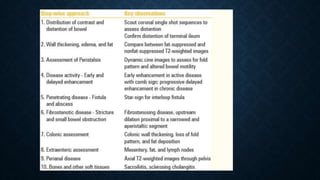
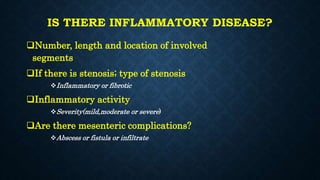
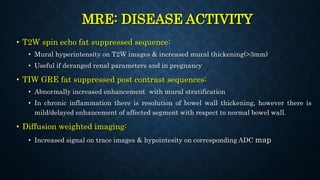
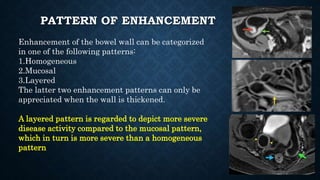
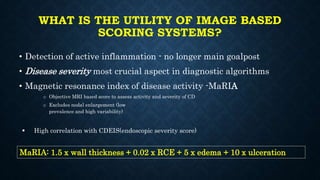
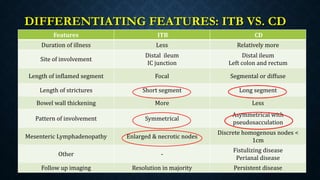
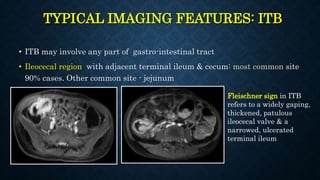
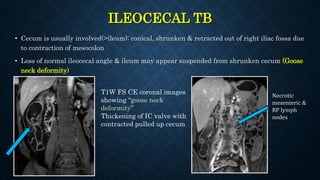
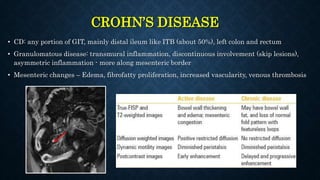
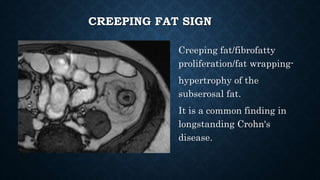
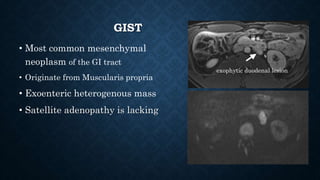
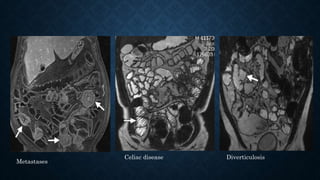
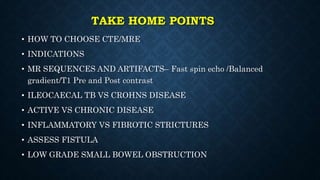
MR enterography/enteroclysis is a non-invasive technique used to diagnose small bowel disorders. Enterography involves oral contrast, while enteroclysis uses a nasoenteric tube. MR enterography offers multiplanar imaging and functional data without radiation. It is superior to CT for assessing peri-anal disease and bowel peristalsis. Indications include Crohn's disease, tuberculosis, and neoplasms. Contrast agents improve luminal visualization. Techniques involve prone positioning, antiperistaltic drugs, and pre- and post-contrast sequences. Findings are used to characterize inflammation, activity, complications and differentiate conditions like tuberculosis from Crohn's disease. Scoring systems like MaRIA objectively assess