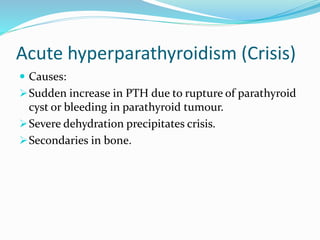
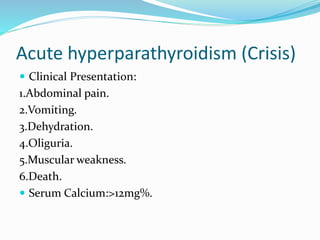
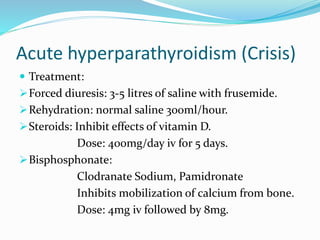
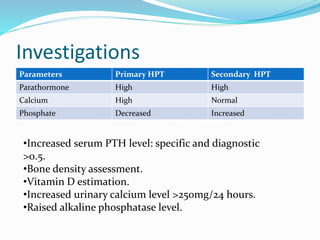
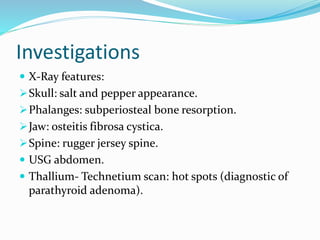
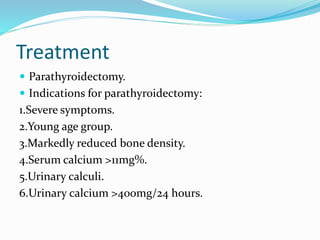
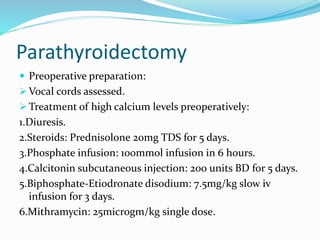
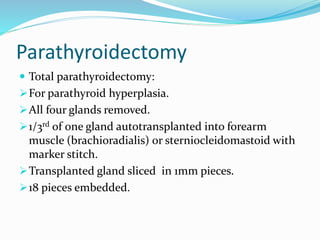
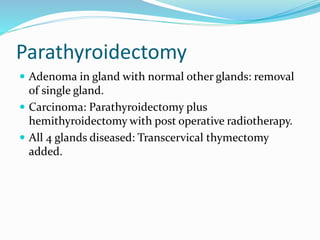
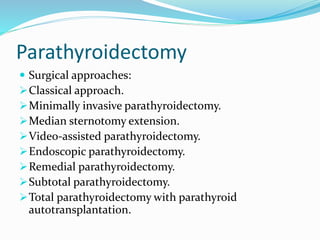
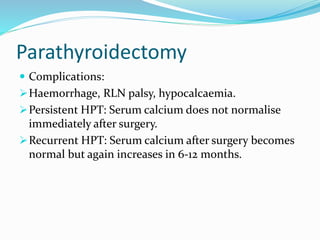
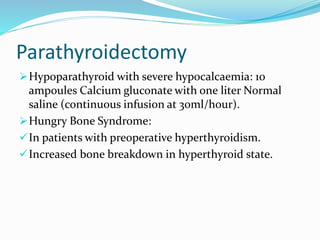
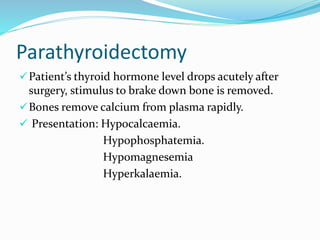
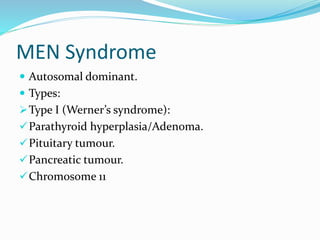
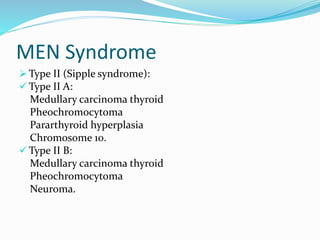
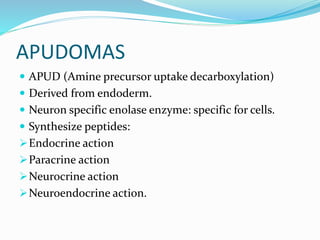
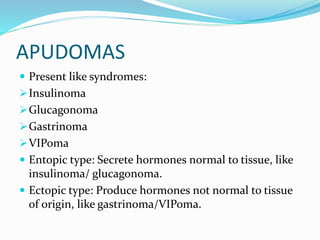
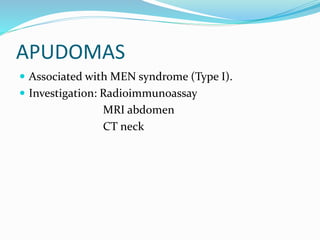
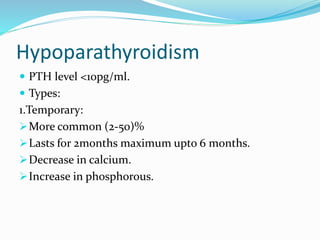
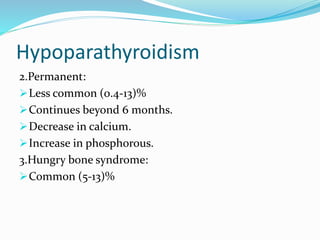
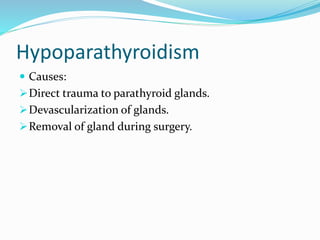
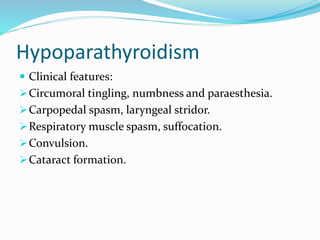
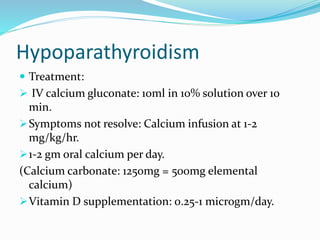
This document provides information on parathyroid glands and parathyroid hormone (PTH). It discusses the anatomy and blood supply of the parathyroid glands. It describes PTH, its functions, and how it regulates calcium levels. It outlines primary hyperparathyroidism, including causes, clinical features, investigations, and treatment via parathyroidectomy. It also briefly discusses secondary and tertiary hyperparathyroidism, acute hyperparathyroidism, MEN syndrome, apudomas, and hypoparathyroidism.