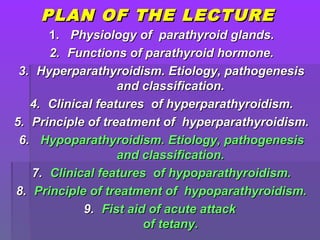
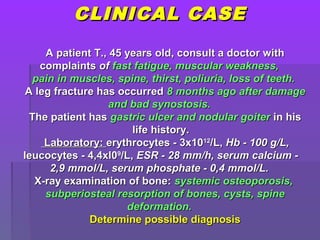
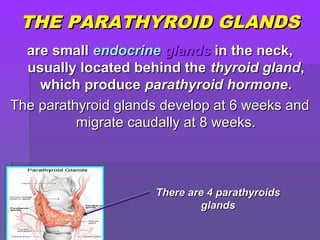
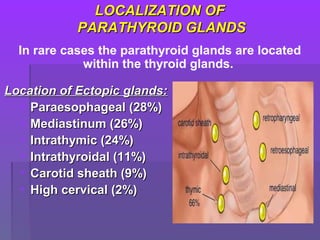
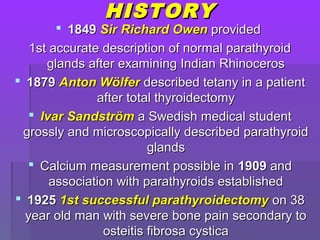
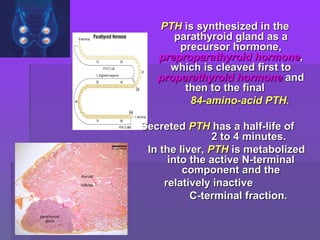
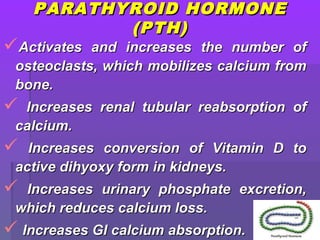
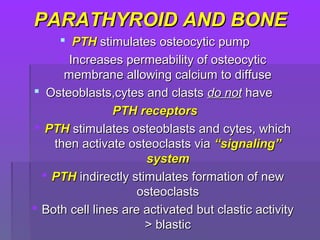
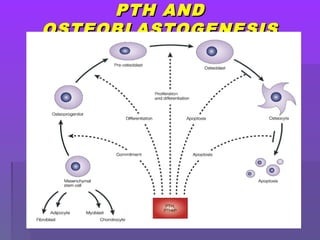
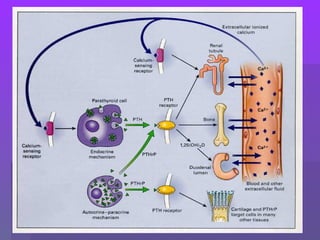
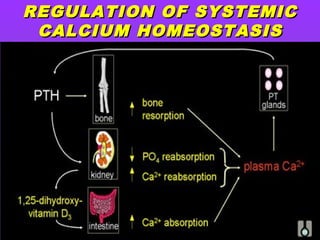
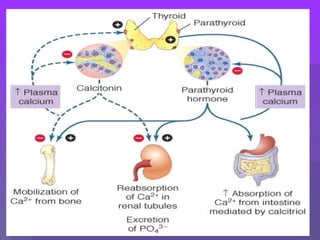
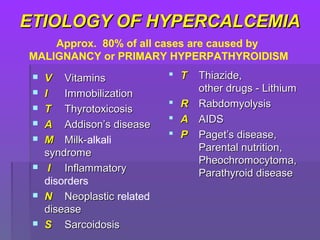
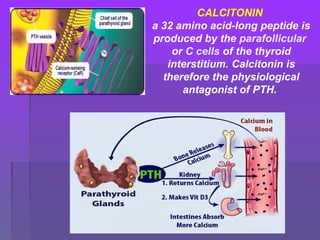
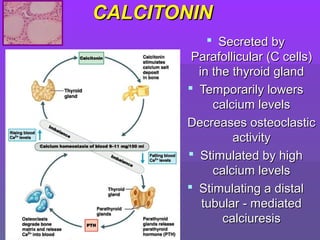
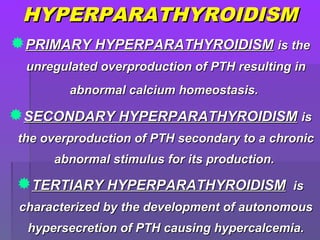
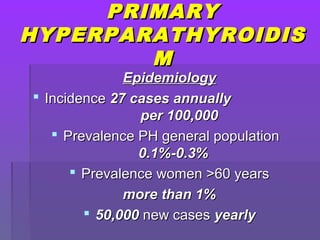
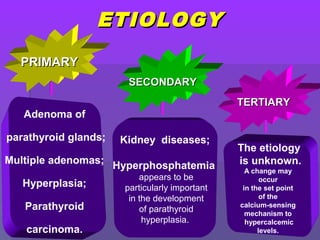
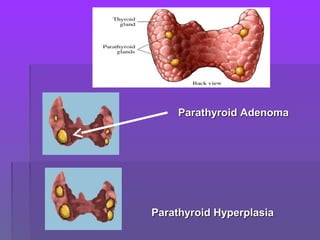
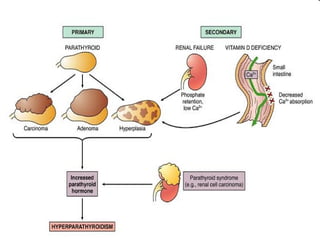
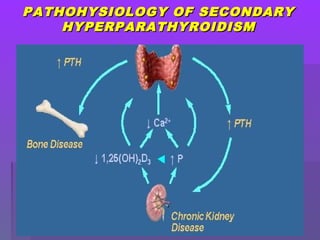
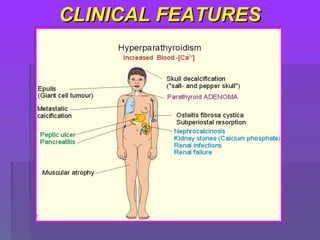
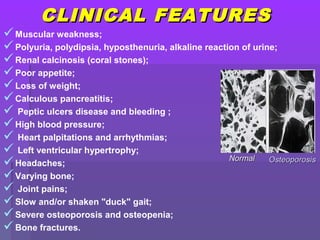
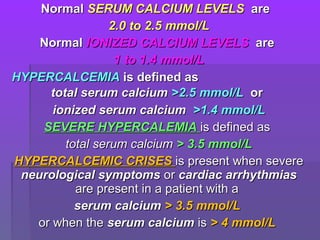
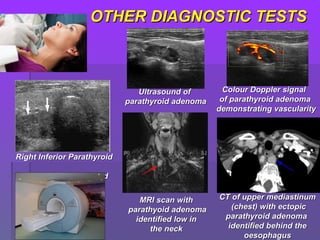
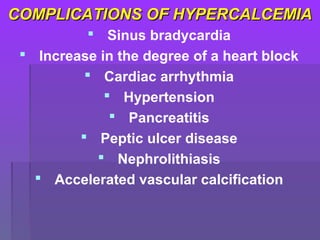
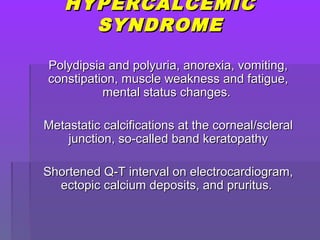
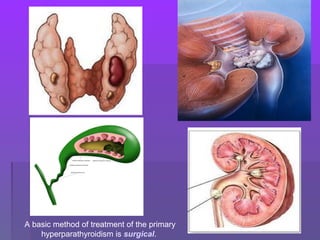
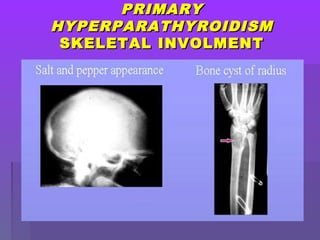
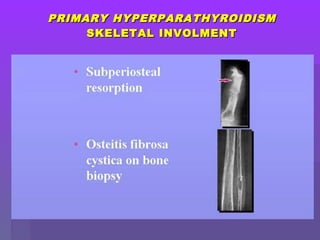
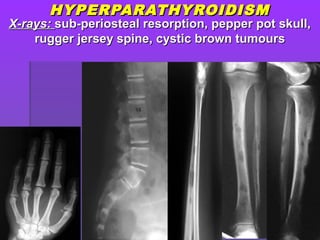
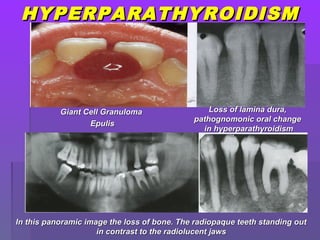
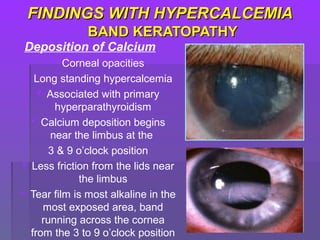
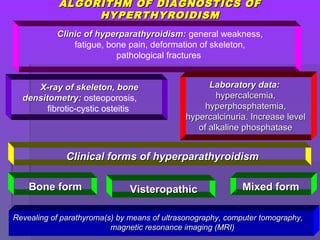
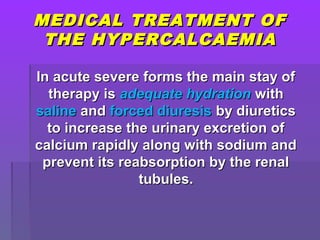
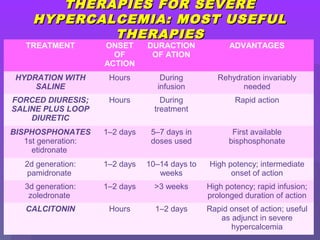
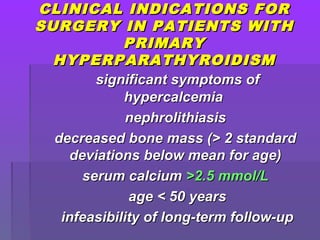
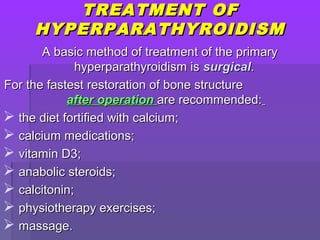
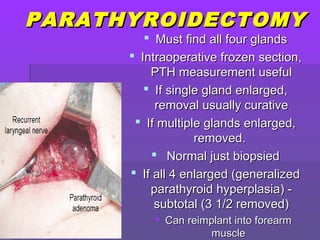
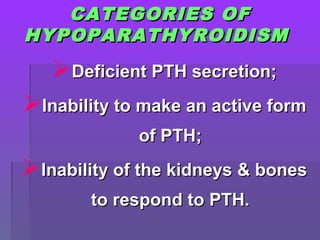
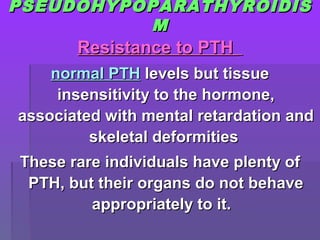
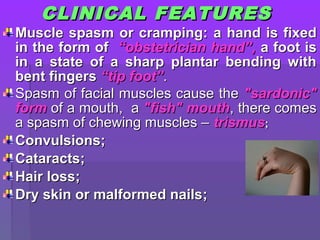
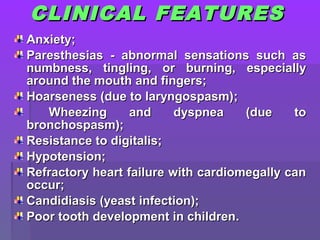
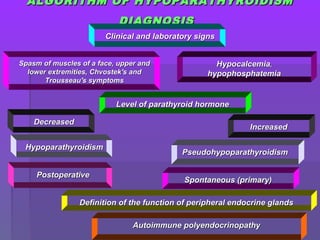
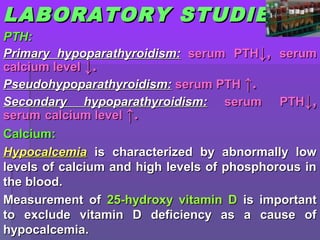
The document discusses diseases of the parathyroid glands, including hyperparathyroidism and hypoparathyroidism. It covers the physiology and functions of the parathyroid glands and parathyroid hormone. It describes the etiology, pathogenesis, and classification of primary, secondary, and tertiary hyperparathyroidism. The clinical features of hyperparathyroidism are also outlined.