The document discusses the benefits of exercise for mental health. Regular physical activity can help reduce anxiety and depression and improve mood and cognitive functioning. Exercise causes chemical changes in the brain that may help protect against mental illness and improve symptoms.
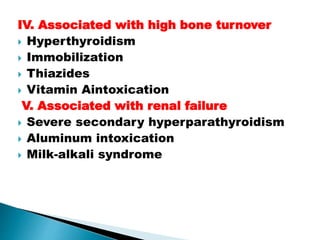
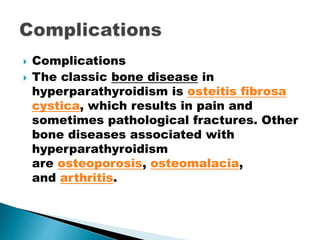
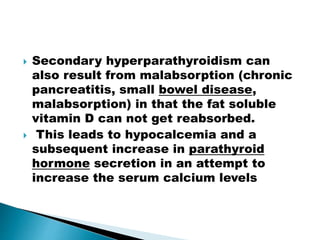
![ "Bones" refers to bone-related
complications. The classic bone disease in
hyperparathyroidism is osteitis fibrosa
cystica, which results in pain and sometimes
pathological fractures. Other bone diseases
associated with hyperparathyroidism
are osteoporosis, osteomalacia, and arthritis.
"Abdominal groans" refers to
gastrointestinal symptoms
of constipation, indigestion, nausea and vomiti
ng.
Hypercalcemia can lead to peptic
ulcers and acute pancreatitis. The peptic
ulcers can be an effect of increased gastric
acid secretion by hypercalcemia,[4] but may
also be part of a multiple endocrine neoplasia
type 1 syndrome of both hyperparathyroid
neoplasia and a gastrinoma.](https://image.slidesharecdn.com/parathyroidppt-150526143032-lva1-app6891/85/Parathyroidppt-20-320.jpg)

![ Physical examination of someone
with hypocalcemia may show tetany, but it is also
possible to provoke tetany of the facial muscles by
tapping on the facial nerve (a phenomenon known
as Chvostek's sign) or by using the cuff of
a sphygmomanometer to temporarily obstruct the
blood flow to the arm (a phenomenon known
asTrousseau's sign of latent tetany).
A number of medical emergencies can arise in people
with low calcium levels. These are seizures, severe
irregularities in the normal heart beat, as well as
spasm of the upper part of the airways or the smaller
airways known as the bronchi (both potentially
causing respiratory failure).[1]](https://image.slidesharecdn.com/parathyroidppt-150526143032-lva1-app6891/85/Parathyroidppt-45-320.jpg)