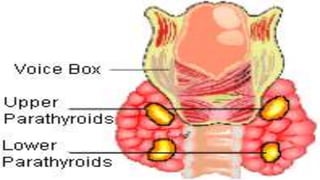
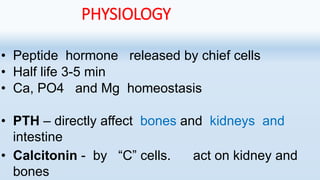
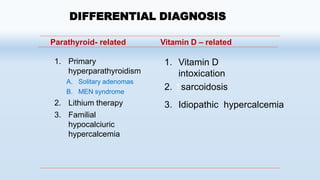
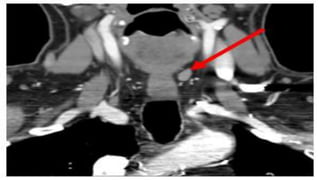
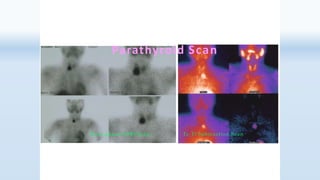
1. Primary hyperparathyroidism is usually caused by a solitary parathyroid adenoma and results in excessive PTH production leading to hypercalcemia.
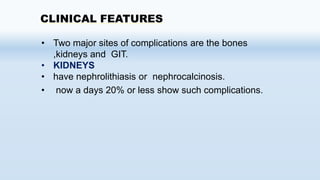
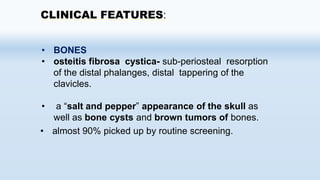
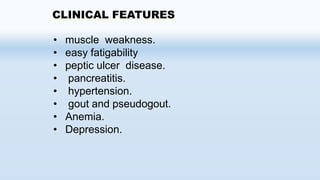
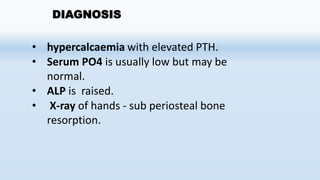
2. Symptoms include kidney stones, bone abnormalities, muscle weakness, and fatigue. Diagnosis is made by detecting hypercalcemia with elevated PTH levels.
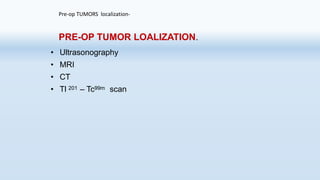
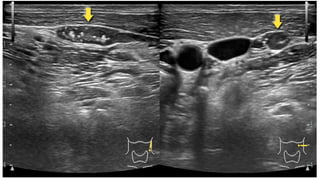
3. Treatment involves surgical removal of the enlarged parathyroid gland.