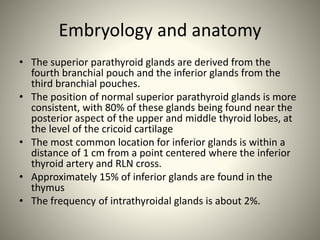
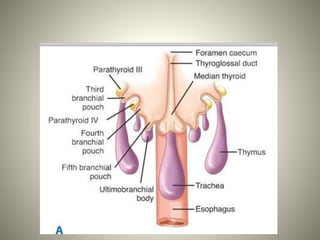
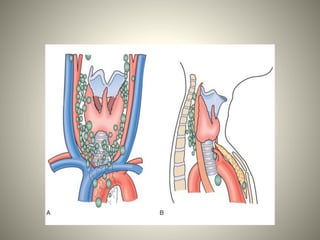
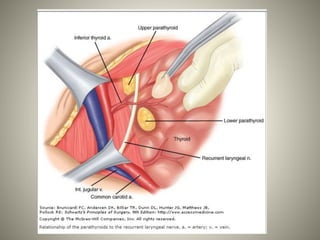
1. The parathyroid glands develop from the third and fourth branchial pouches during embryology. There are typically four parathyroid glands in adults, with the superior glands usually located near the thyroid and the inferior glands located lower in the neck.
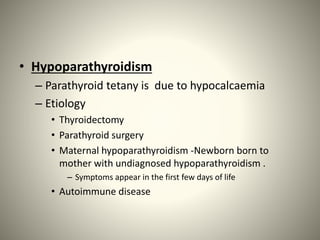
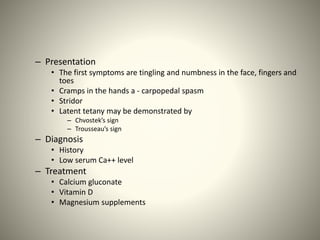
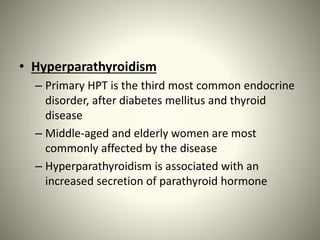
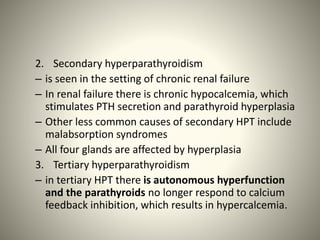
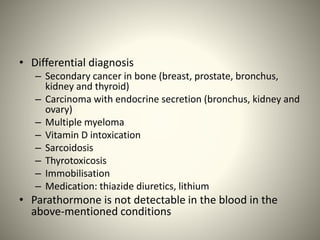
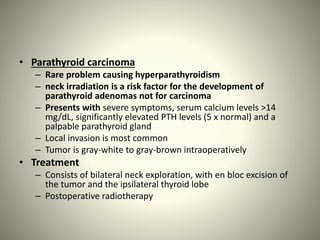
2. Parathyroid disorders include hypoparathyroidism caused by low calcium levels and hyperparathyroidism caused by excessive PTH levels. Primary hyperparathyroidism is usually due to a benign adenoma and presents with increased calcium levels.
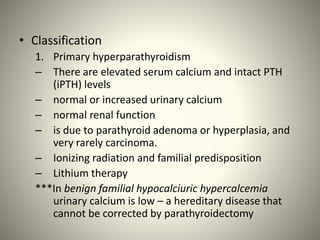
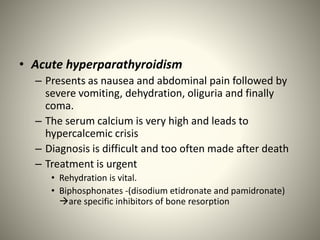
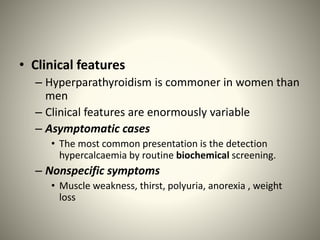
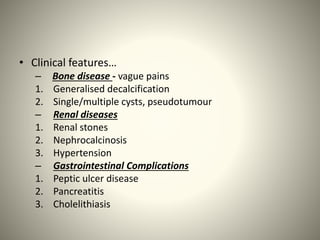
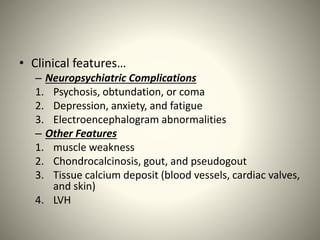
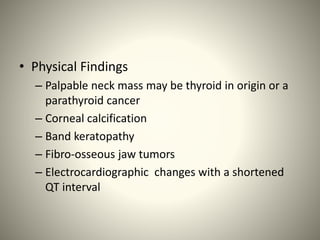
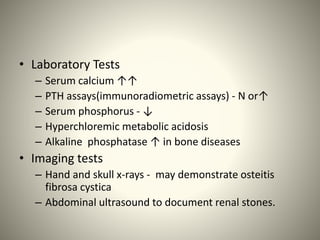
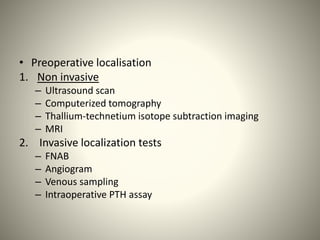
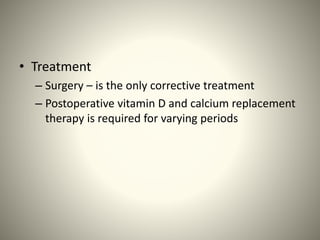
3. Symptoms of hyperparathyroidism range from being asymptomatic to musculoskeletal and renal problems. Diagnosis involves blood tests showing elevated calcium and PTH levels. Treatment is surgical