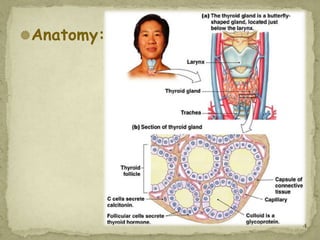
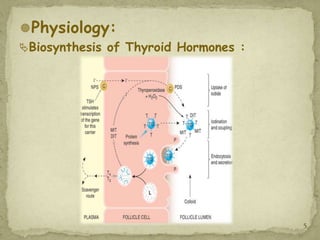
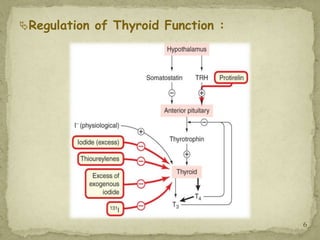
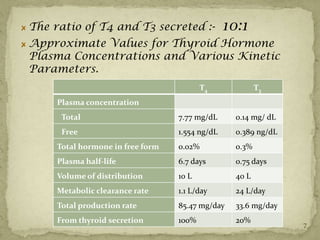
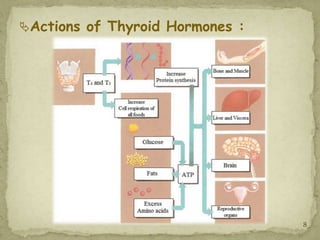
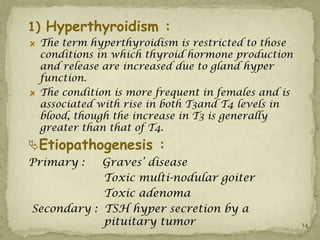
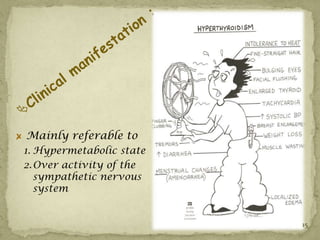
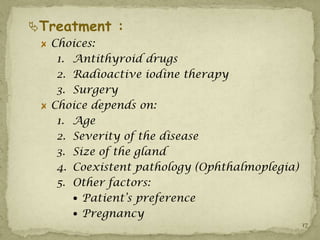
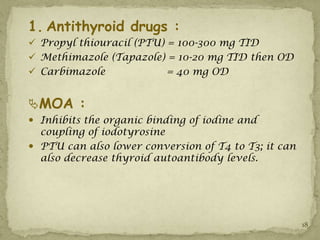
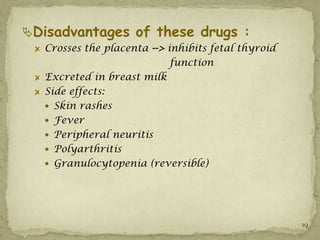
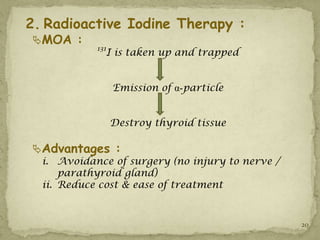
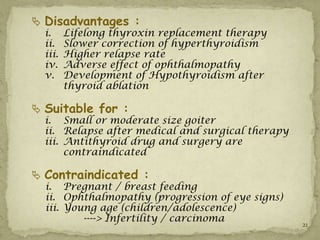
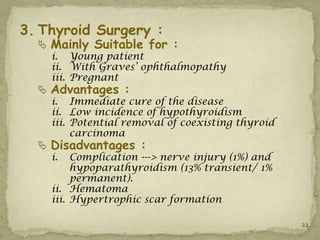
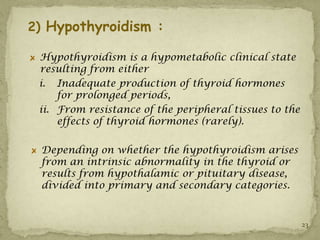
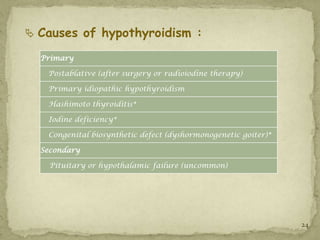
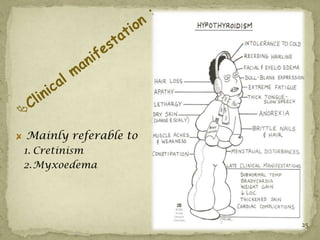
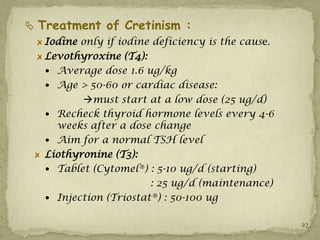
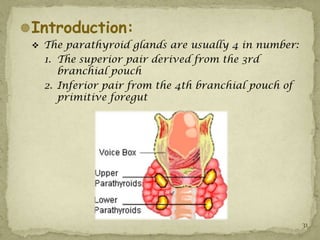
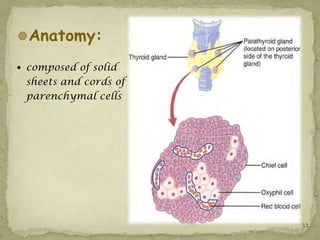
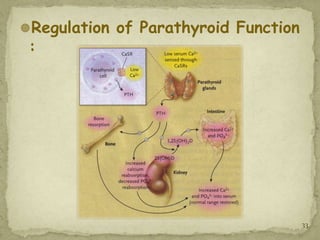
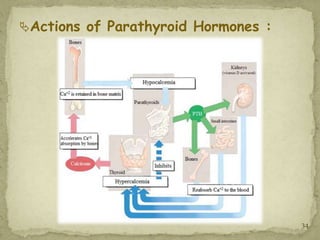
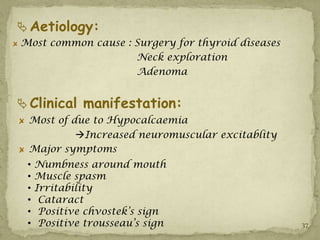
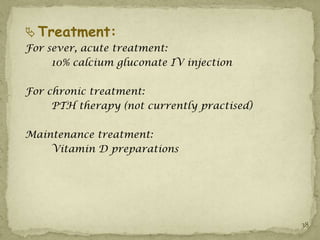
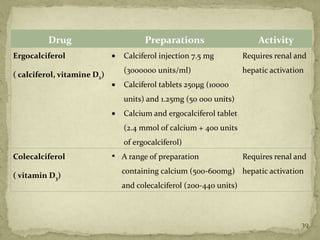
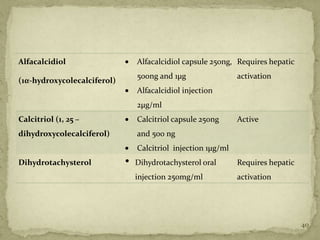
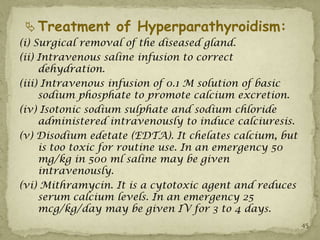
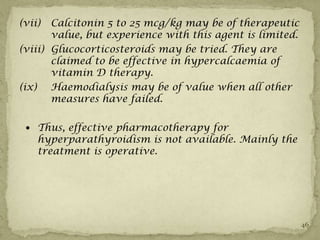
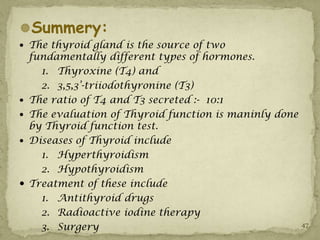
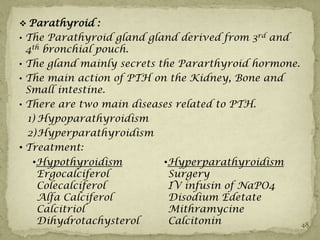
The document summarizes information about the thyroid and parathyroid glands. It discusses the anatomy, physiology, diseases and treatment of hypothyroidism and hyperthyroidism. It also covers the anatomy, regulation, actions and diseases including hypoparathyroidism and hyperparathyroidism of the parathyroid glands. Evaluation and management of thyroid and parathyroid disorders is outlined.