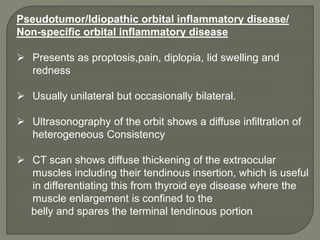
This document discusses orbital cellulitis and its causes, signs, symptoms, investigations, differential diagnosis, treatment and complications. Some key points:
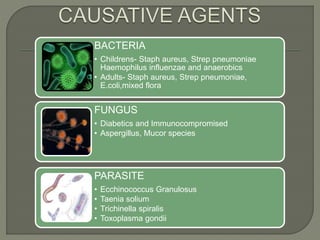
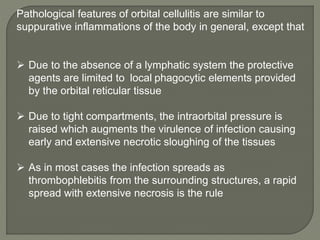
- Orbital cellulitis is an infection of the soft tissues of the eyelids and orbit. It is usually caused by Staphylococcus aureus or Streptococcus bacteria spreading from nearby infections.
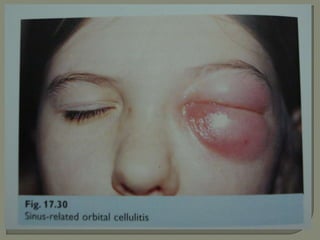
- Symptoms include eyelid swelling, pain, redness and fever. Proptosis and vision issues may occur if the infection spreads to the orbit.
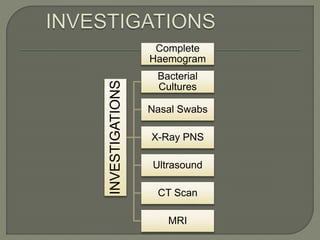
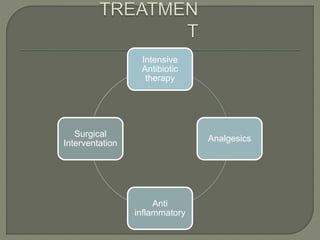
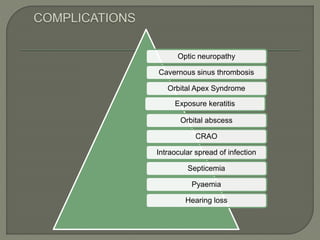
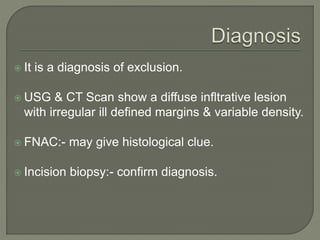
- Diagnosis involves examination, blood tests and imaging like CT scans. Broad-spectrum antibiotics are the primary treatment. Surgery may be needed to drain abscesses. Complications can include vision loss, ca