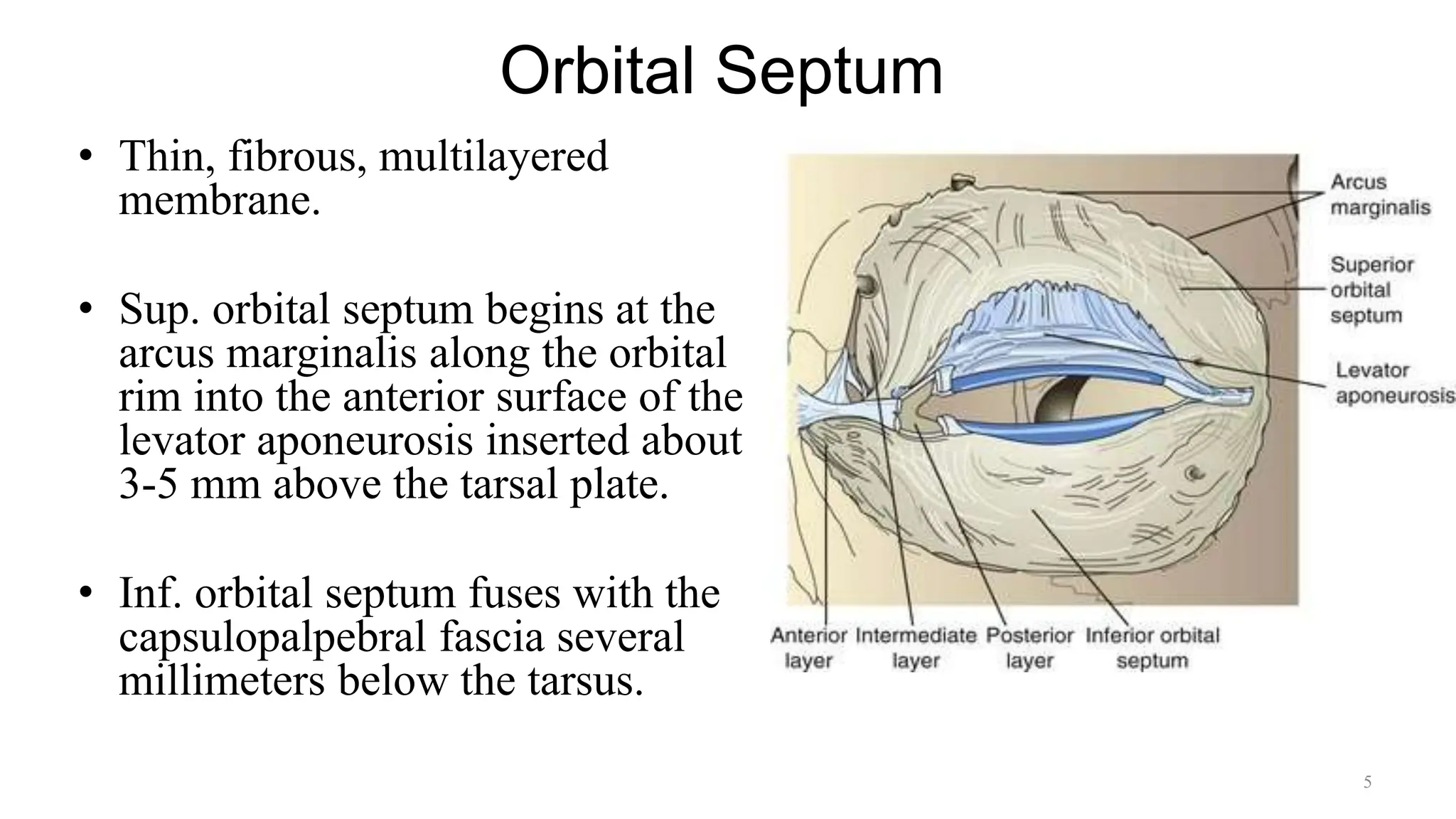
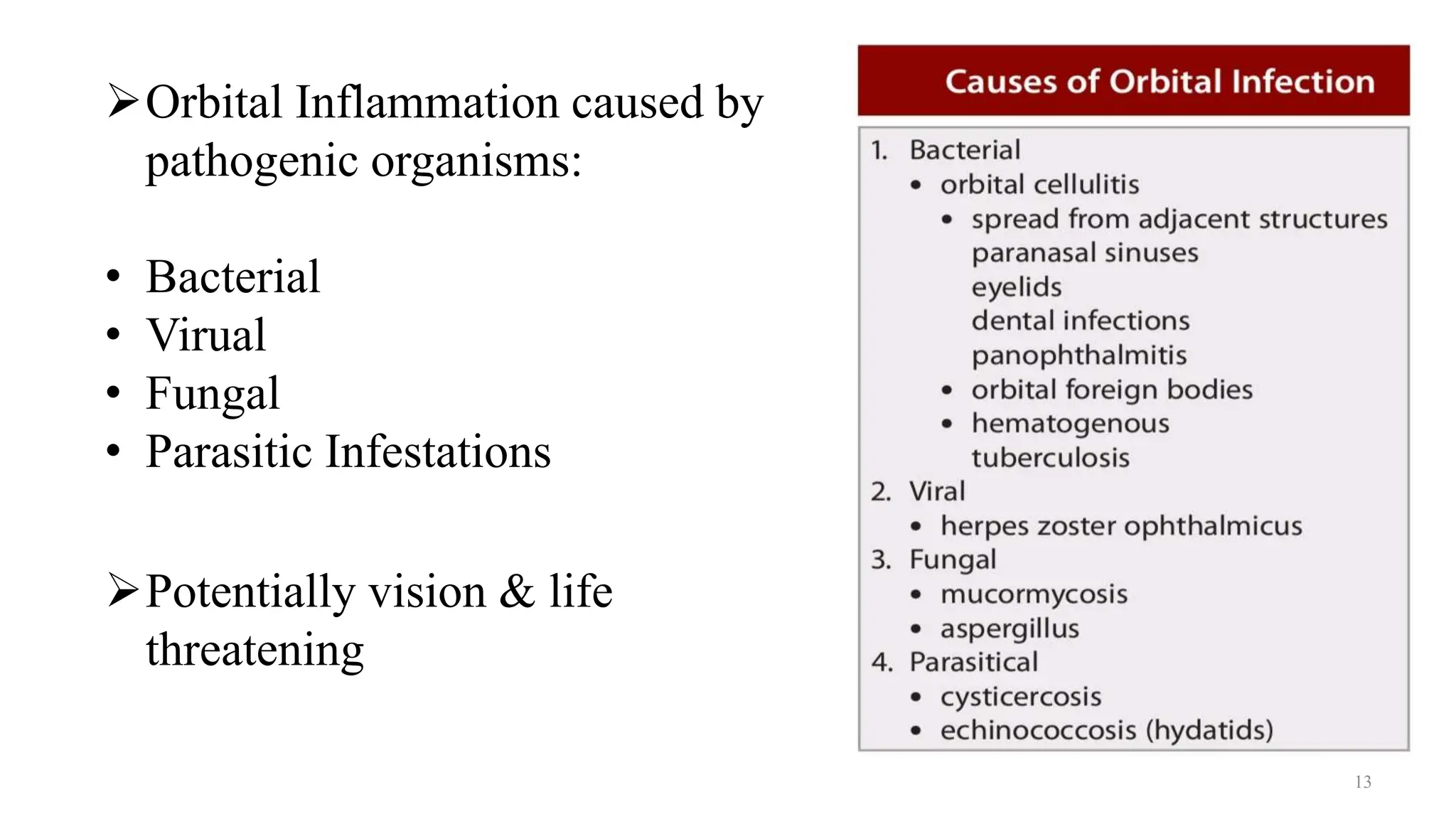
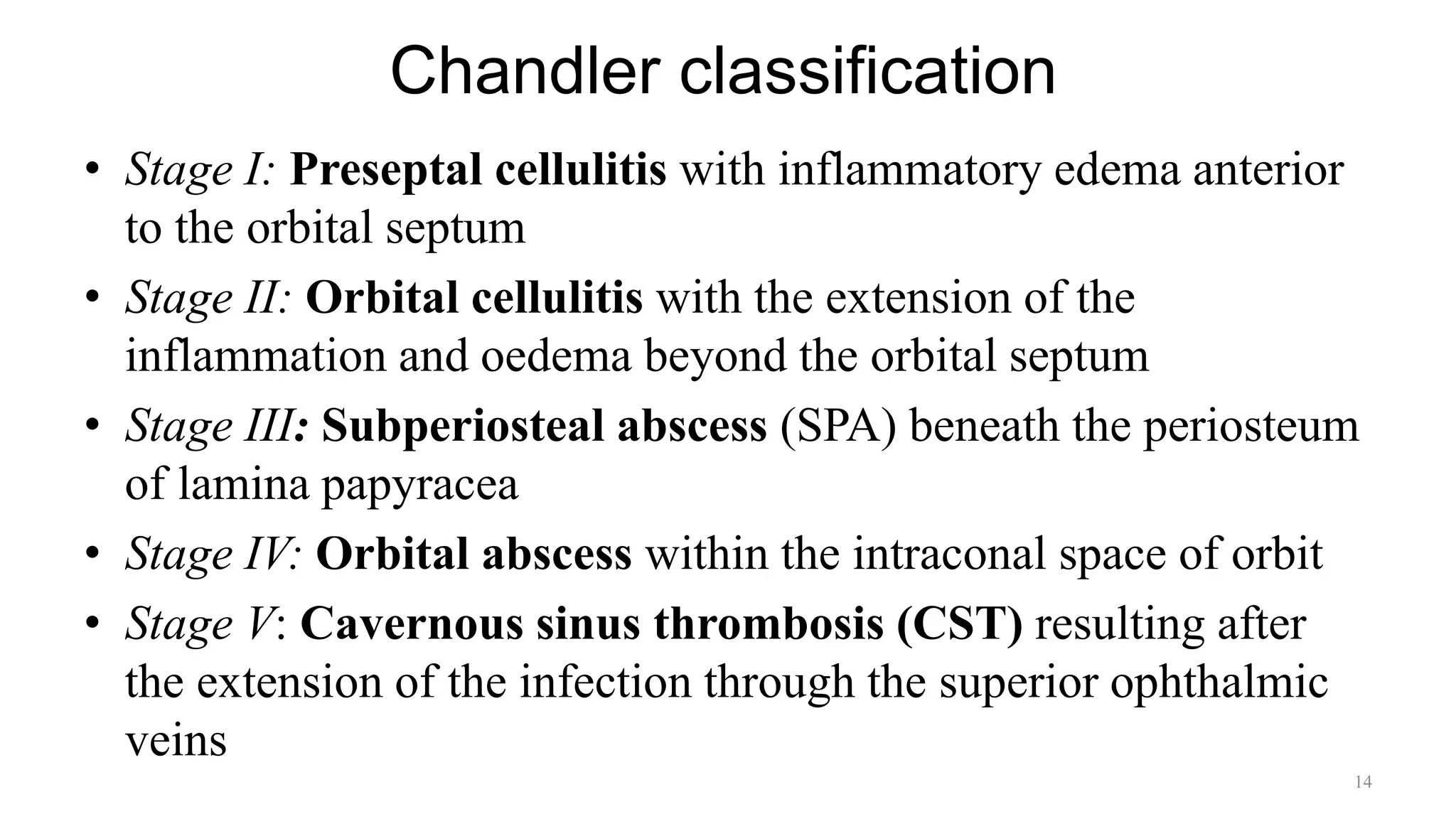
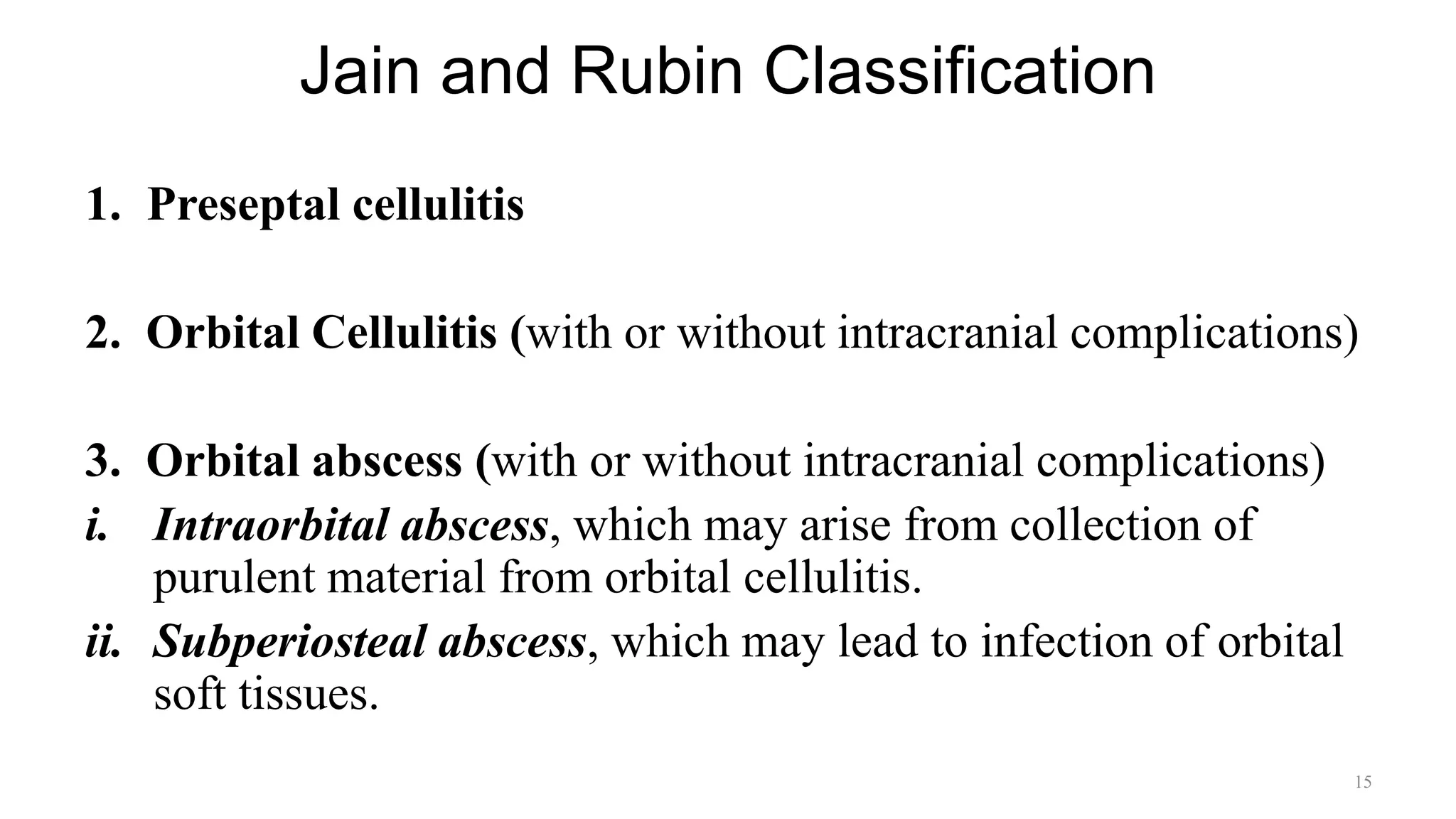
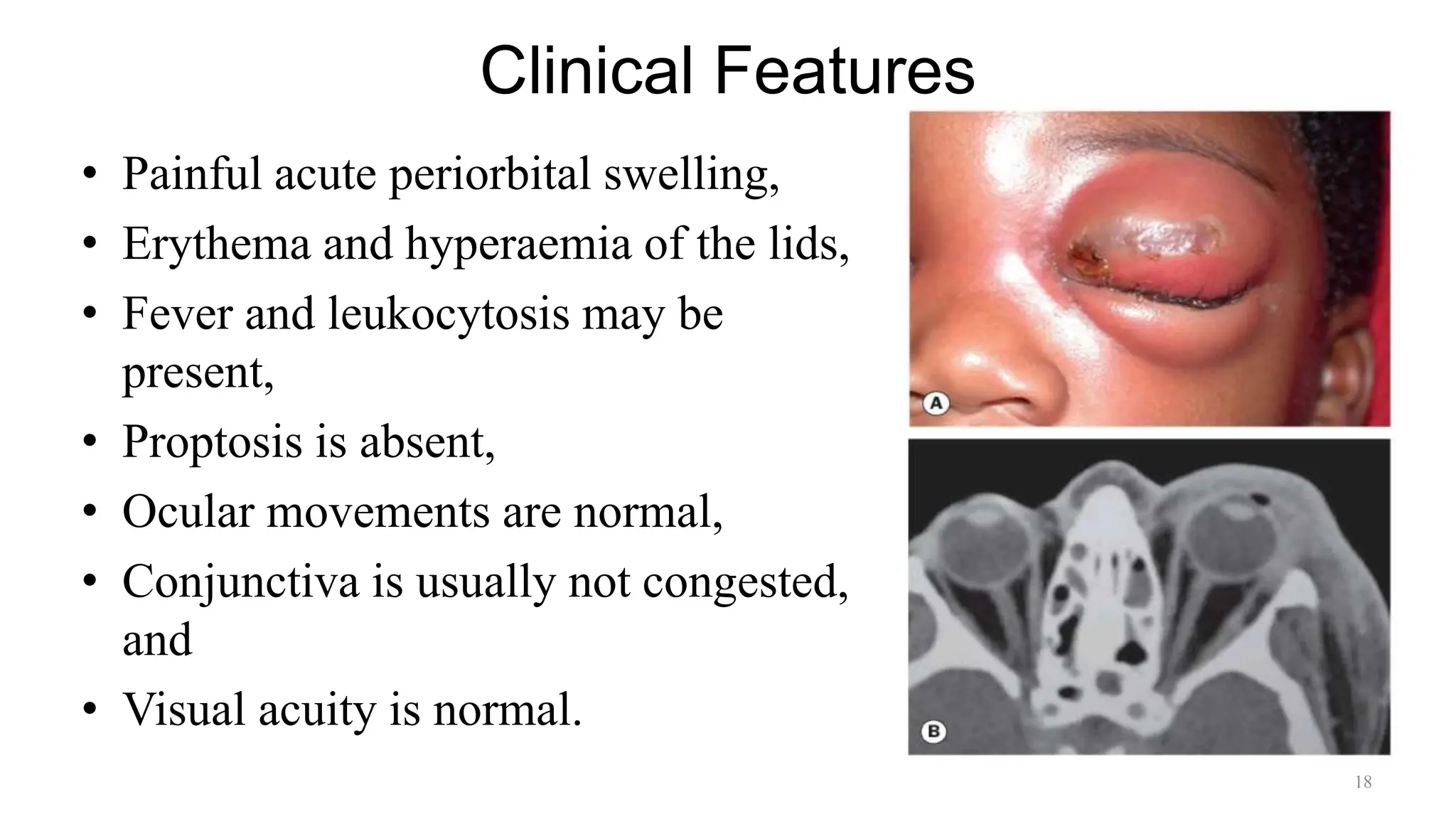
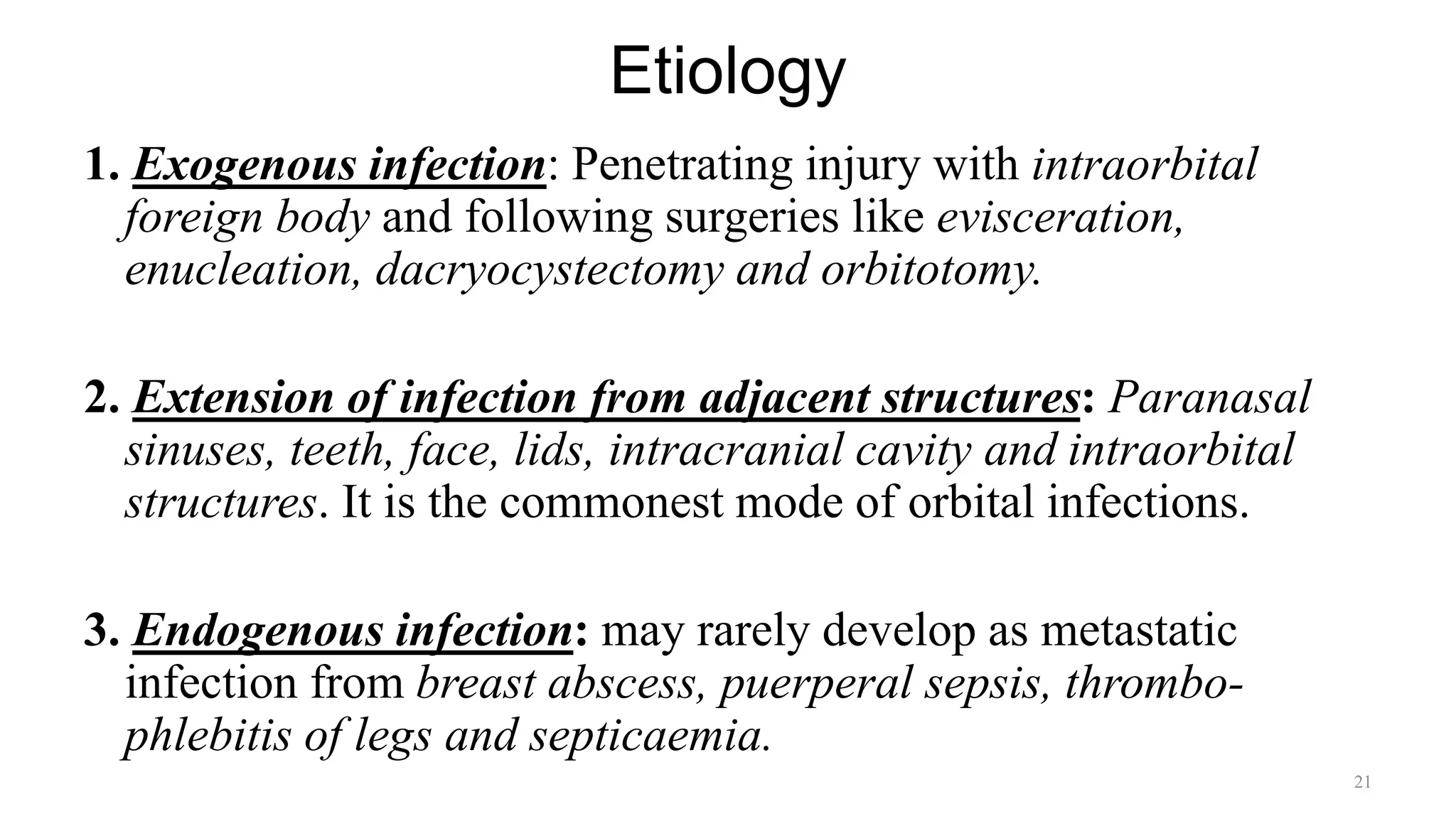
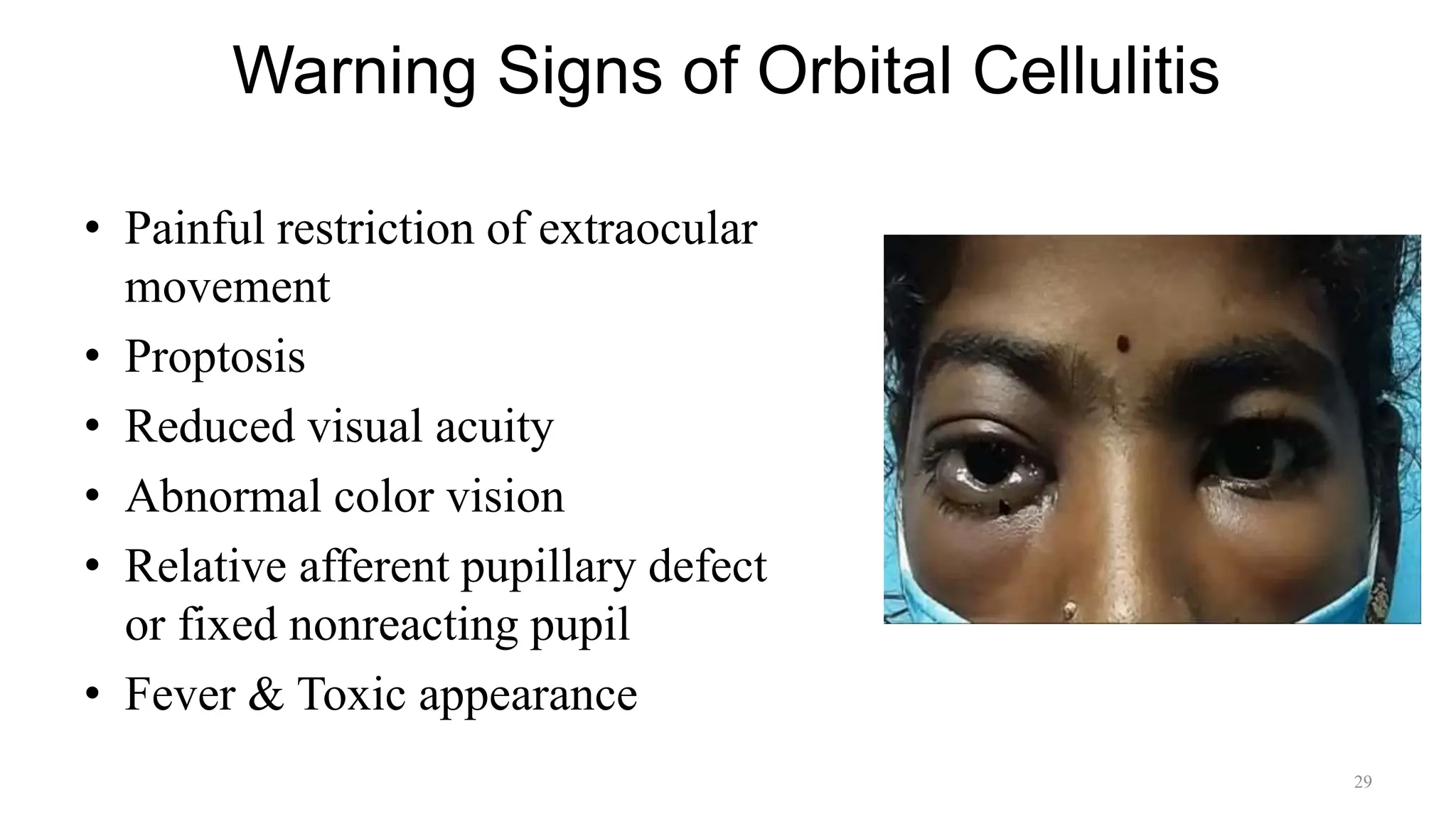
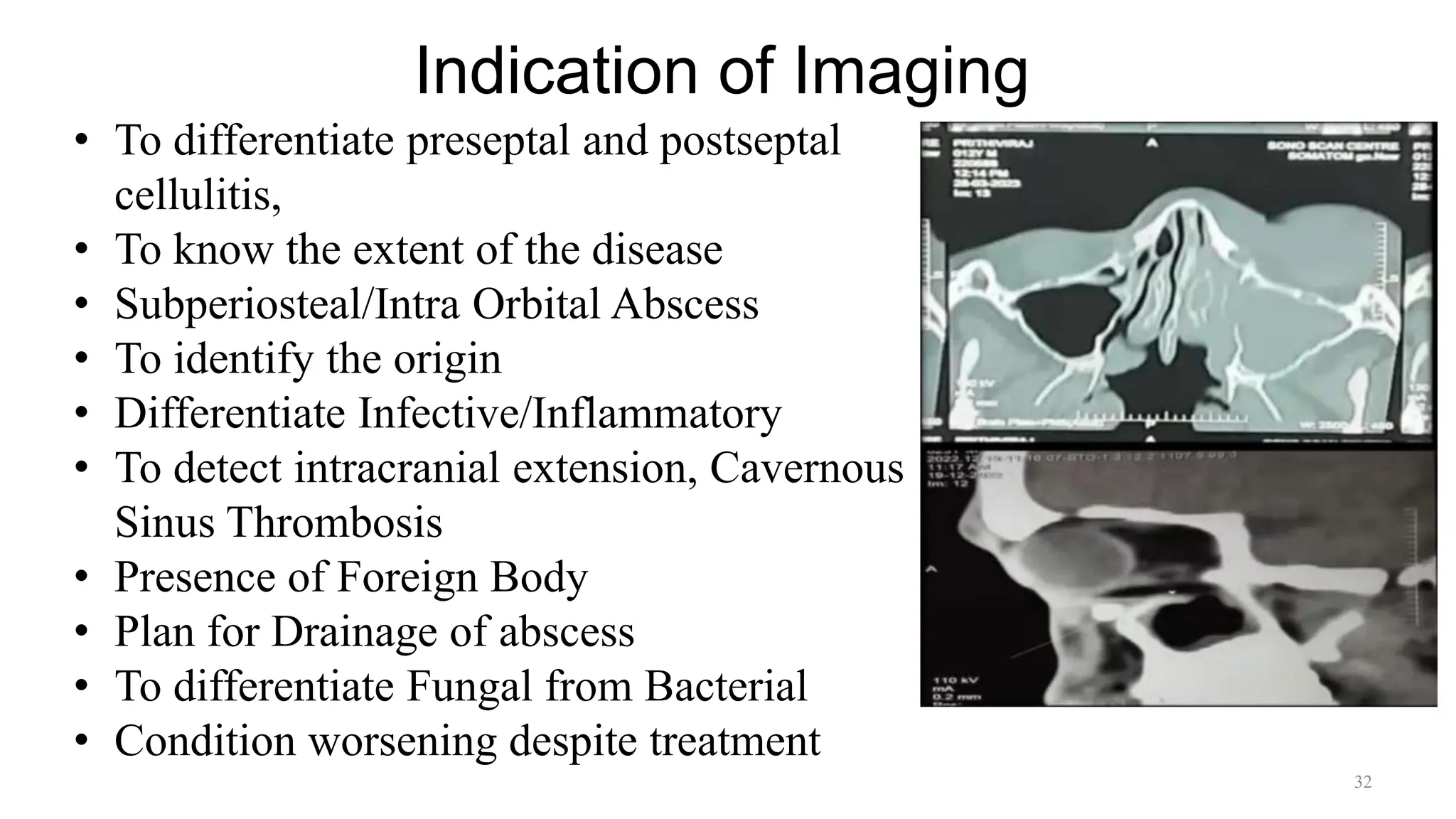
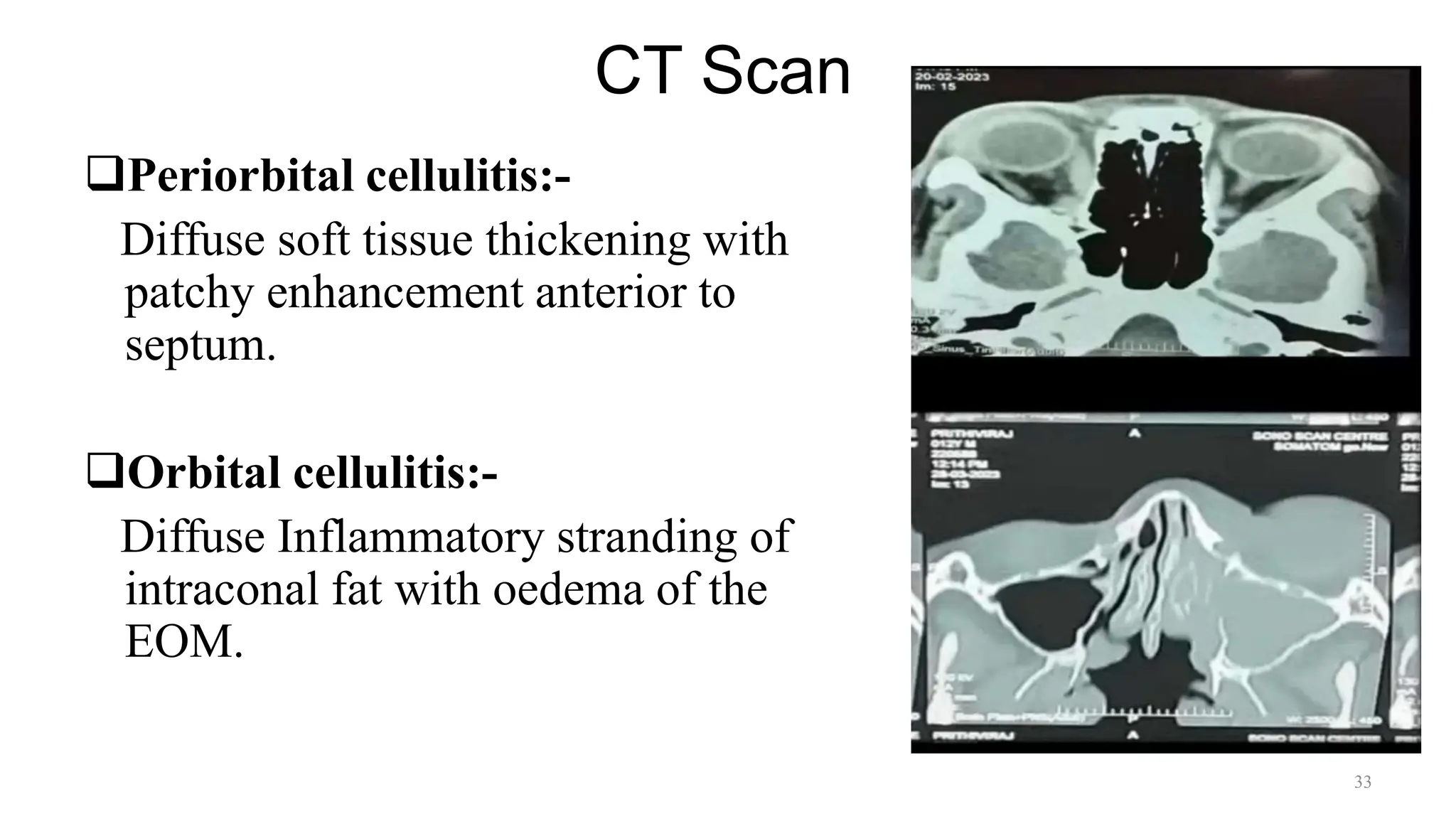
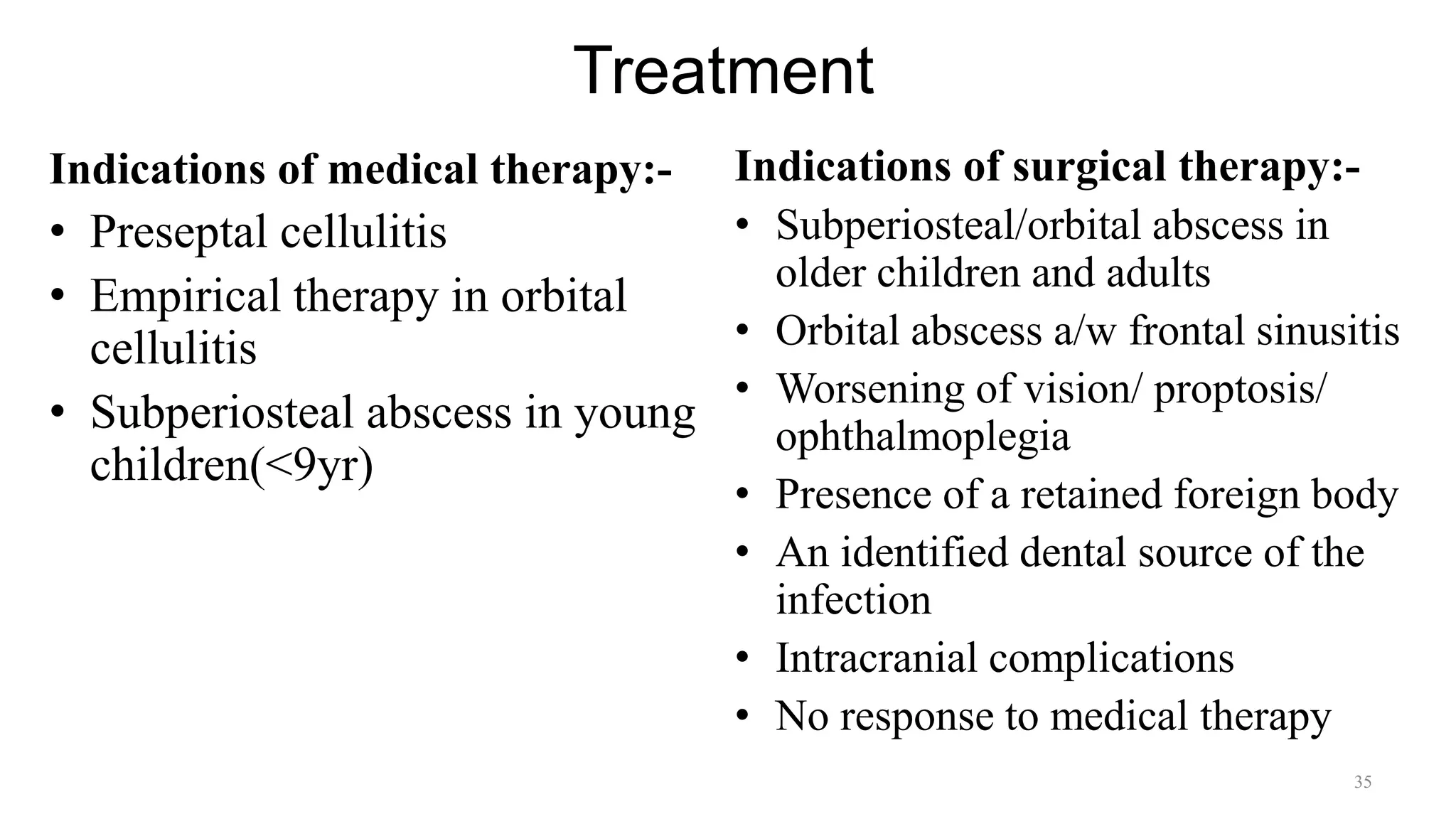
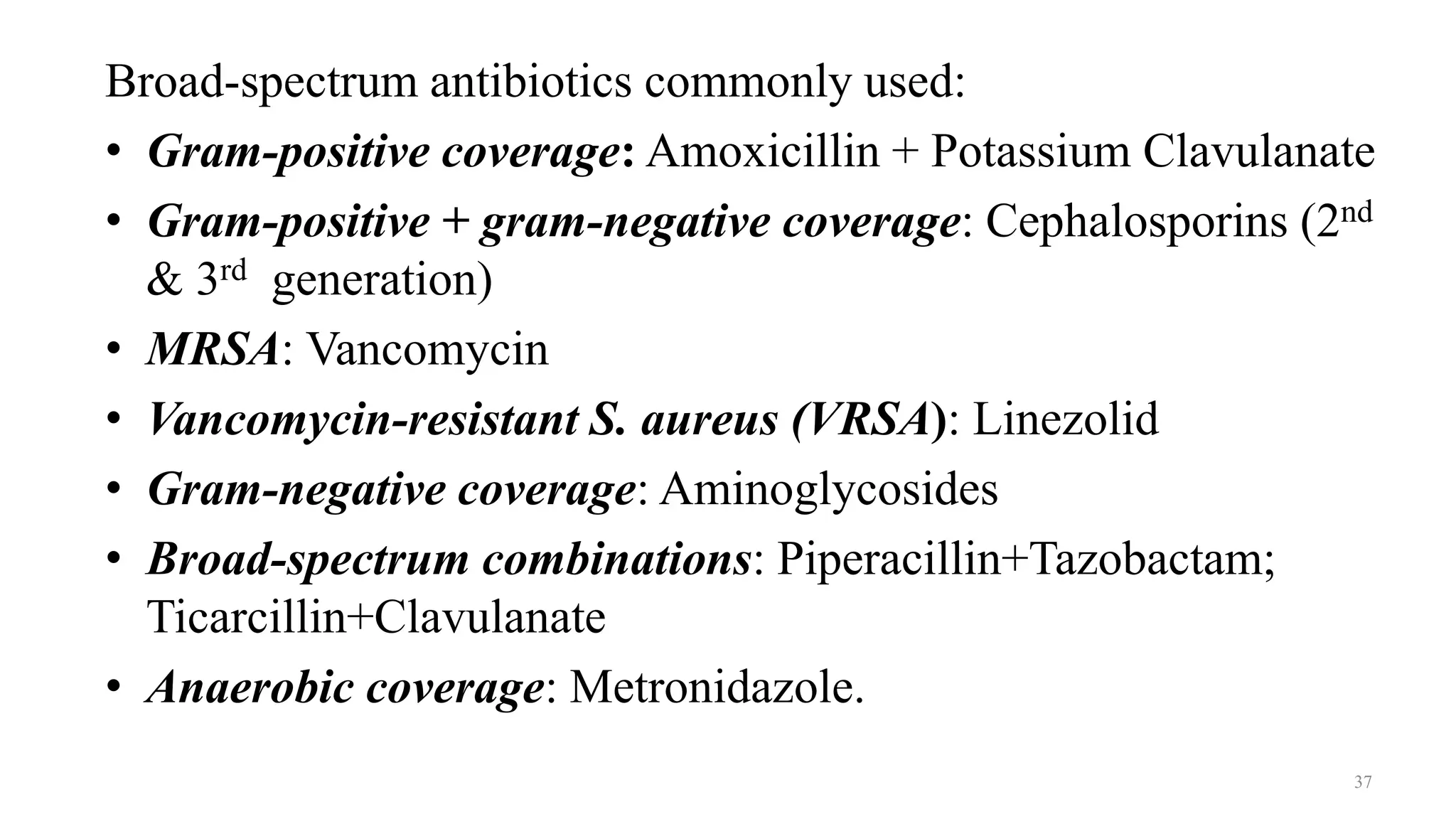
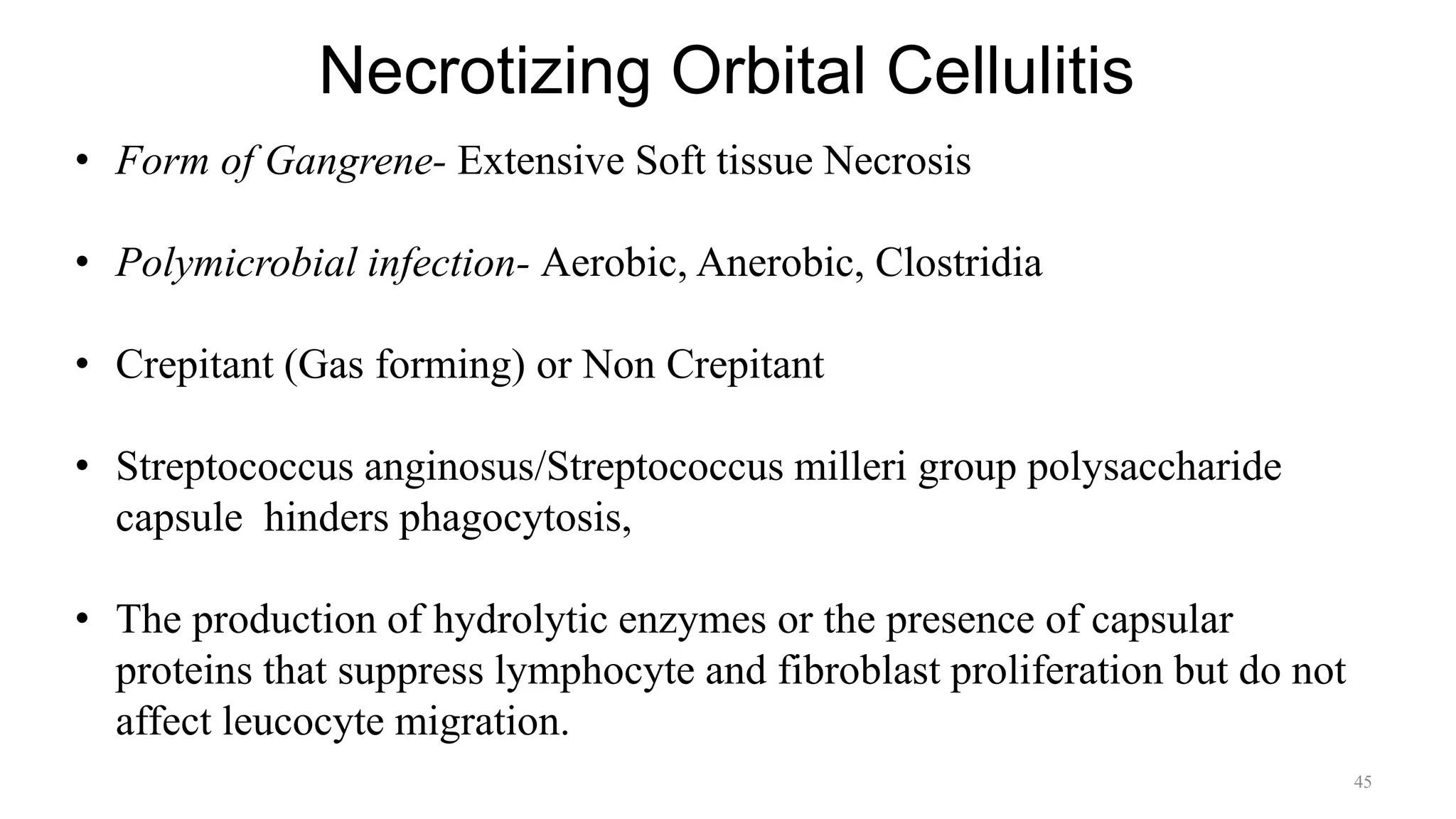
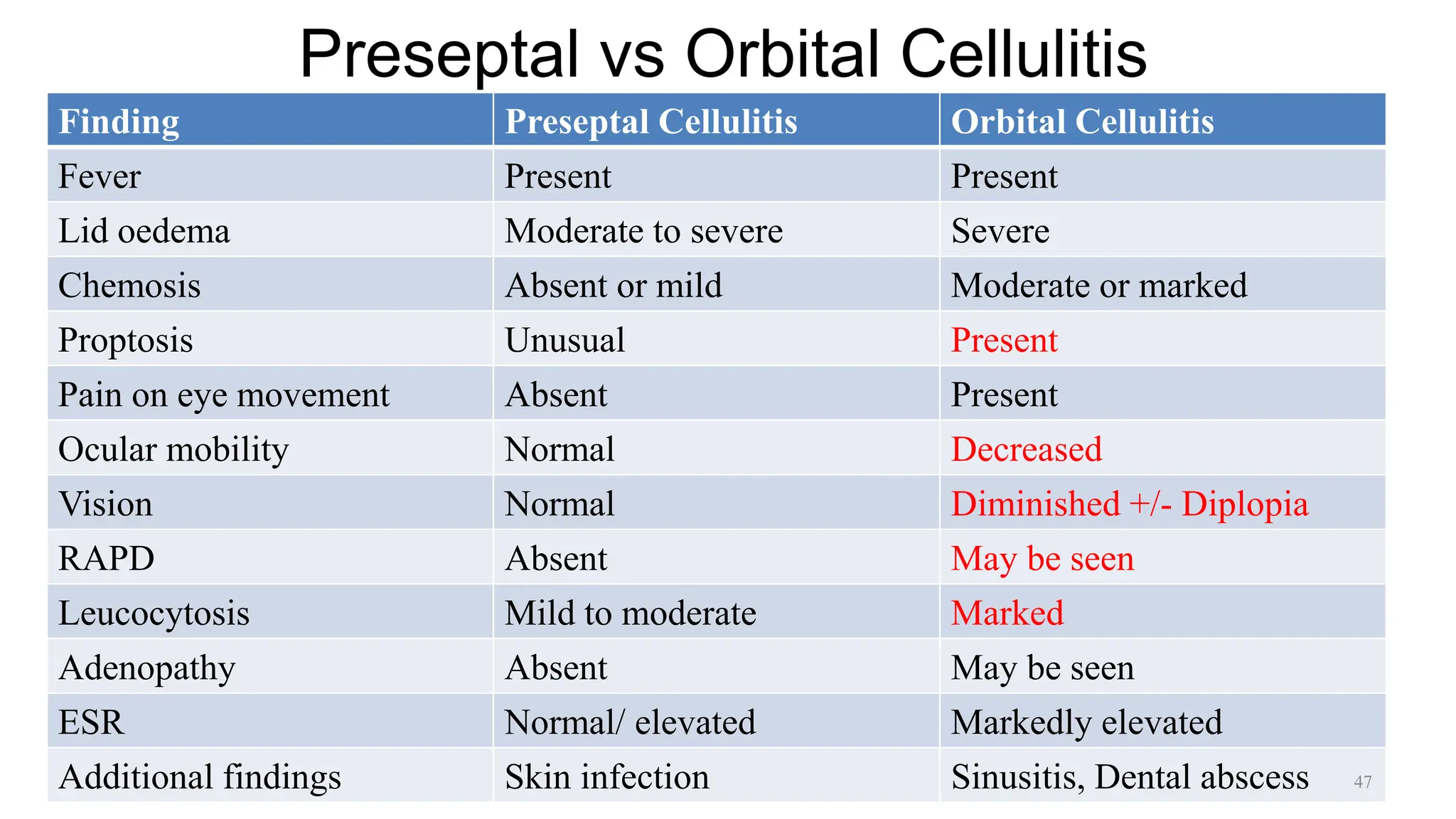
The document provides a comprehensive overview of infections in the orbit, focusing on preseptal and orbital cellulitis, their anatomy, pathophysiology, and treatment options. It categorizes different stages of infections based on severity and outlines clinical symptoms, diagnostic criteria, and emergency management approaches. Various causative organisms are discussed, along with the necessary interventions for effective treatment and potential complications associated with these infections.