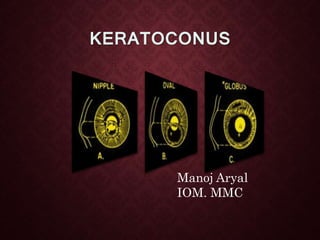
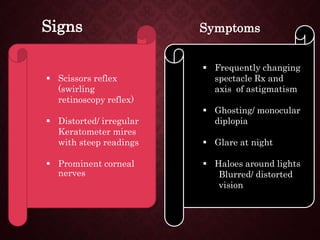
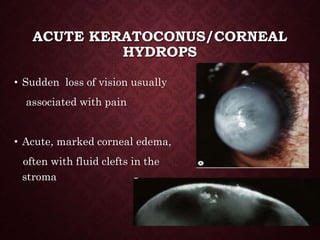
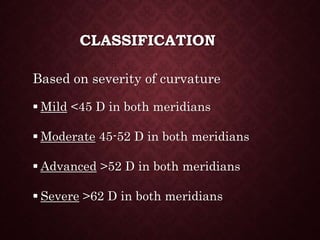
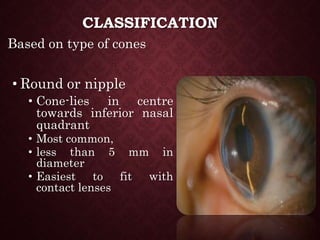
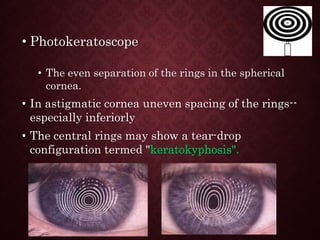
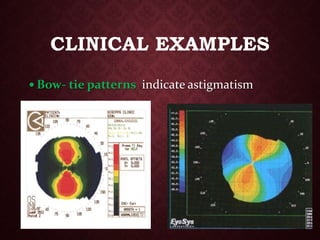
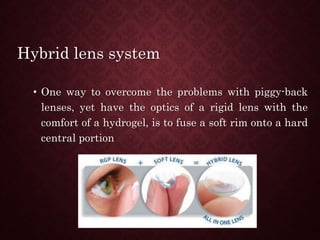
This document provides an overview of keratoconus, including its etiology, signs and symptoms, classification, and management. Keratoconus is a non-inflammatory thinning of the cornea that results in a cone-shaped protrusion and irregular astigmatism. It typically onset in teenagers and progresses over time. Management includes rigid gas permeable contact lenses, collagen cross-linking to halt progression, and keratoplasty for advanced cases.