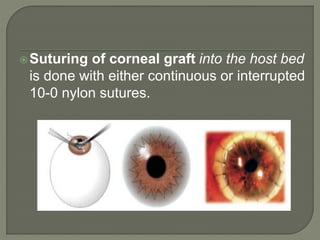
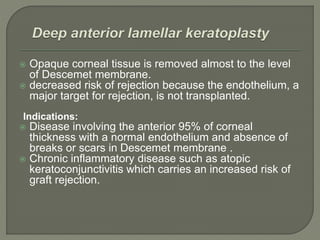
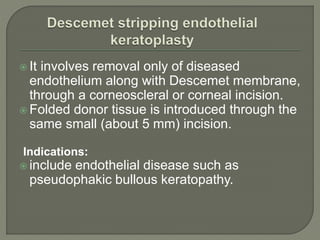
This document discusses corneal transplantation, including definitions, types (penetrating keratoplasty and lamellar keratoplasty), indications, donor evaluation and storage, contraindications, surgical techniques, and postoperative care and complications. It provides details on penetrating keratoplasty, including that it is the most common type and its main indications are diseases involving all corneal layers. It also summarizes anterior and posterior lamellar keratoplasty.