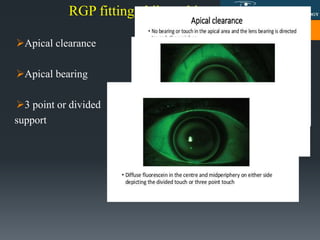
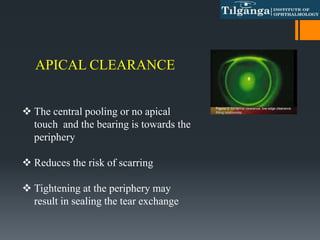
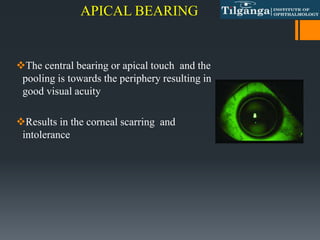
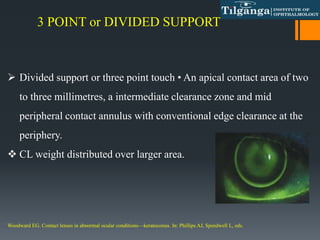
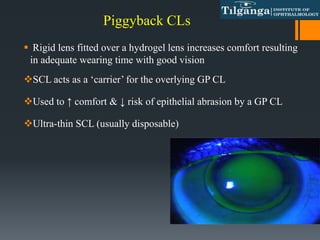
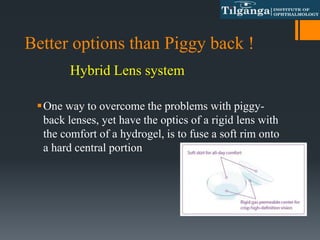
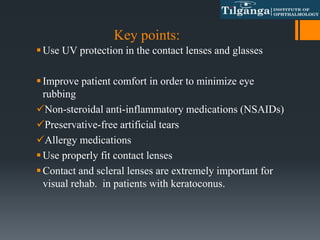
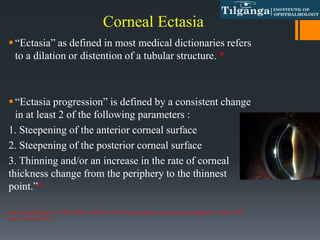
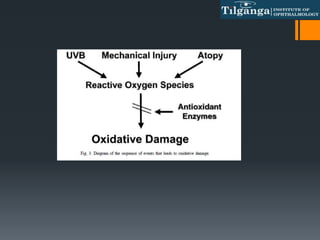
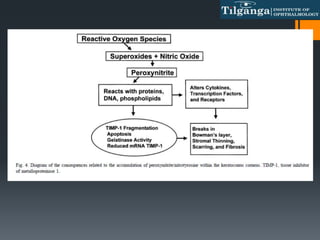
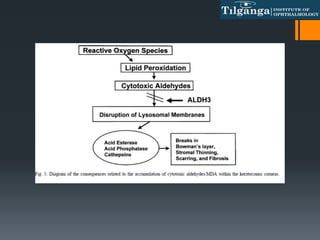
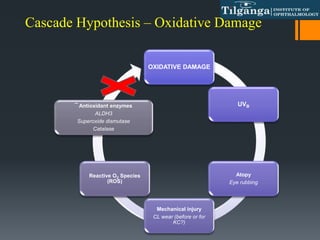
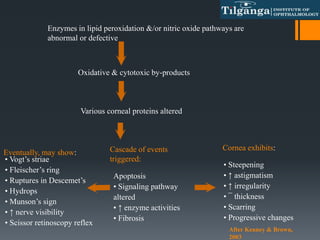
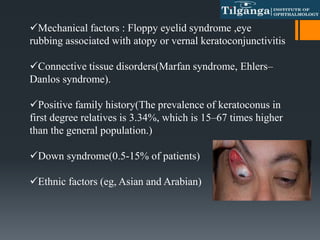
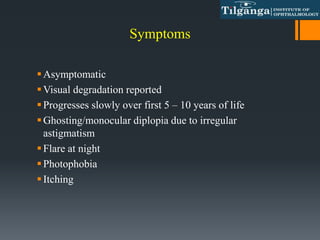
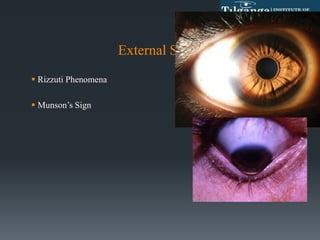
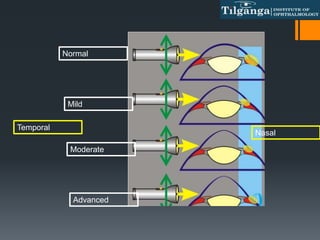
This document discusses ectatic disorders of the cornea, focusing on keratoconus. It defines keratoconus as a non-inflammatory thinning of the cornea that results in a protrusion and irregular astigmatism. The document covers the cascade hypothesis of oxidative damage in keratoconus pathogenesis, classification systems for keratoconus severity, signs and symptoms, and non-surgical management approaches like spectacles, contact lenses, and RGP fitting philosophies. The goal of management is to eliminate irregularities and provide optimal vision correction while minimizing further corneal damage.


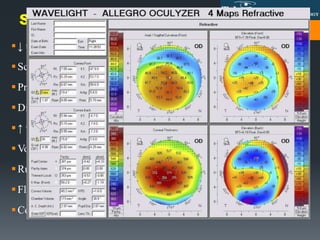
![KISA%: Rabinowitz Criteria
Corneal power (K) [>47.2 D]
Inferior-Superior dioptric asymmetry (I-S) [>1.2 D]
Sim K Astigmatism (Ast) >1.5 D
Skewed Radial Axis (SRAX) [>21°]
If KISA% > 60%, case is a KC suspect
KISA = (Central K) × (I−S) × (AST) × (SRAX) × 100/300](https://image.slidesharecdn.com/keratoconus-copy-210823144217/85/Keratoconus-and-Its-management-34-320.jpg)